

Biomaterial kept mesenchymal stem cells alive and considerably reduced the size of the lesion caused by stroke in a study involving mice. The procedure could help repair brain areas in even larger lesions (images reproduced by courtesy of the researchers)
Biomaterial kept mesenchymal stem cells alive and considerably reduced the size of the lesion caused by stroke in a study involving mice. The procedure could help repair brain areas in even larger lesions.
Biomaterial kept mesenchymal stem cells alive and considerably reduced the size of the lesion caused by stroke in a study involving mice. The procedure could help repair brain areas in even larger lesions.
Biomaterial kept mesenchymal stem cells alive and considerably reduced the size of the lesion caused by stroke in a study involving mice. The procedure could help repair brain areas in even larger lesions (images reproduced by courtesy of the researchers)
By André Julião | Agência FAPESP – Researchers have succeeded in using stem cells to reduce the size of lesions caused by strokes in the brains of mice.
Mesenchymal stem cells, which can differentiate into various tissues, were extracted from the bone marrow and cultured on scaffolds made of a material that not only permitted their survival and multiplication but also prevented their migration to other brain areas, a process that frequently occurs when stem cells are added directly to lesions.
The technique could be used to help ischemic stroke victims recover. Acute ischemic stroke is caused by the thrombotic blockage of a cerebral artery followed by neuronal death in the part of the brain that is deprived of blood flow. It can have serious consequences, including loss of movement and the eventual death of the patient.
Two procedures are currently used to treat ischemic stroke patients. One is endovascular recanalization therapy (thrombolysis), which involves the administration of drugs that dissolve blood clots by activating plasminogen. The other is the use of a catheter to access the clot and remove it manually to restore normal blood flow.
These procedures are effective only if they take place within four and a half hours of the stroke, after which time cell death is irreversible. The new technique offers a chance to intervene at a later time.
The results of the study have been published in an article in Nanomedicine: Nanotechnology, Biology, and Medicine, with Laura Zamproni as the first author. The study was part of her PhD research, which was supported by a scholarship from FAPESP at the Federal University of São Paulo’s Medical School (EPM-UNIFESP) in Brazil, where she is currently doing postdoctoral research.
Zamproni is a neurologist at Hospital São Paulo, which also belongs to UNIFESP. Her day-to-day work aroused her interest in basic scientific research. “The procedures currently used to treat ischemic stroke have their benefits, but even when they are performed as quickly as necessary, they can have complications and may cause cognitive deficits,” she said.
This was not the first time scientists had tried using stem cells to repair brain damage in mice or rats. In previous trials involving the direct delivery of stem cells to lesions, however, almost none of the cells survived (less than 0.005%), and even those that survived migrated to other brain regions. When stem cells were injected into the bloodstream, they were retained in the kidneys or lungs.
What made the difference in this study was the use of a scaffold that is biocompatible (nontoxic), enhances the stem cell survival rate and ensures that the cells stay in the lesion, reducing inflammation. Some months later, when the lesion has mostly been repaired, the scaffold is fully absorbed by the organism.
The innovation was developed by biomedical engineers Anderson de Oliveira Lobo and Fernanda Roberta Marciano. Both are affiliated with Universidade Brasil and were awarded grants under FAPESP’s Young Investigator program.
The material they developed for use as a scaffold is a highly porous organic polymeric rough microfiber made of polylactic acid and produced by rotary jet spinning in a process similar to that by which cotton candy is made.
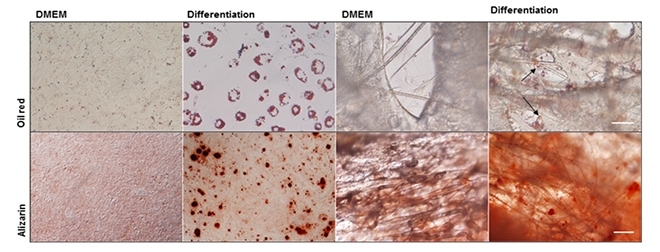
In the study, mesenchymal stem cells were extracted from murine bone marrow and cultured on coverslips or scaffolds.
“When this material containing the mesenchymal stem cells was implanted into a lesioned brain, the lesion decreased to one-third of its size without any intervention,” said Marimélia Porcionatto, a professor at EPM-UNIFESP and principal investigator for the study.
“Previously, we’d performed several tests to confirm that the cells retained biological characteristics such as differentiation and proliferation. This is important, as we can’t use a scaffold material that alters key cell properties,” Porcionatto said.
The fibers containing stem cells were placed over the lesion and monitored for 30 days. The researchers found that the stem cells adapted better to the material than to laboratory culture plates.
Tests showed that the stem cells produced more of a cytokine called CXCL12, which attracts cells to the region. In addition, they produced more integrins, proteins that keep stem cells anchored in the right place.
“It’s as if the mesenchymal stem cells were producing a suitable environment for themselves,” Porcionatto said. “We don’t know what causes this in the material, but it’s very interesting to see how a nonbiological material affects cell behavior.”
The researchers plan to test the stem cell implant technique to treat cranioencephalic trauma with loss of part of the brain.
“At present when there’s loss of encephalic mass we control the bleeding and operate but what’s lost is lost. Nothing can be done to replace it. Our findings suggest a new treatment is possible,” Zamproni said.
The researchers want to use bioprinting to reconstruct the lost part of the brain with a 3D printer. To this end, they are looking for a biomaterial that has the same properties as polylactic acid and can be molded.
The article “Rotary jet-spun porous microfibers as scaffolds for stem cells delivery to central nervous system injury” (doi: 10.1016/j.nano.2018.08.014) by Laura N. Zamproni, Marco A. Grinet, Mayara V. Mundim, Marcella B. Reis, Layla T. Galindo, Fernanda R. Marciano, Anderson O. Lobo and Marimelia Porcionatto is available at: www.sciencedirect.com/science/article/pii/S1549963418305203.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





