

Research conducted with mice in Brazil used different combinations of tumor cell lines genetically modified to secrete substances that stimulate the immune system to combat cancer (image: Frontiers of Immunology)
Research conducted with mice in Brazil used different combinations of tumor cell lines genetically modified to secrete substances that stimulate the immune system to combat cancer.
Research conducted with mice in Brazil used different combinations of tumor cell lines genetically modified to secrete substances that stimulate the immune system to combat cancer.
Research conducted with mice in Brazil used different combinations of tumor cell lines genetically modified to secrete substances that stimulate the immune system to combat cancer (image: Frontiers of Immunology)
By Karina Toledo | Agência FAPESP – By combining genetically modified tumor-derived cell lines, scientists in Campinas (São Paulo State, Brazil) have achieved promising results in the treatment of tumors in mice. The aim of the research, which is supported by FAPESP, is to develop a vaccine that stimulates the human immune system to combat cancer.
The research is being done at the National Bioscience Laboratory (LNBio), attached to Brazil’s National Energy & Materials Research Center (CNPEM). It is part of the PhD research of Andrea Johanna Manrique Rincón, supervised by Marcio Chaim Bajgelman.
“We tested several combinations of genetically modified tumor-derived cell lines. Some entirely prevented the tumor from growing,” Bajgelman told Agência FAPESP. “The results suggest the anti-tumor response induced by the treatment is long-lasting, which would be useful to prevent relapses.”
Many groups around the world have pursued the development of a cancer vaccine, he explained, ever since William B. Coley (1862-1936), a US surgeon, performed experiments with anti-tumor vaccines derived from microorganisms in the early twentieth century.
The most well-established model is GVAX, a cancer vaccine consisting of tumor cells taken from the patient being treated (autologous), genetically modified to secrete the immune stimulatory cytokine GM-CSF (granulocyte-macrophage colony stimulating factor), and then irradiated to prevent uncontrolled proliferation in the organism.
“GVAX has been tested in a murine tumor model in which [unmodified] melanoma cells are injected into the tail vein. Tumors grow in the lungs and cause death in about 28 days. GVAX [applied after the disease has been induced] halted progression and increased the life expectancy of the challenged animals,” Bajgelman said.
Although GVAX has produced promising results in rodents, its success has not been matched in trials with human patients.
The cytokine GM-CSF used in GVAX is considered an immunomodulator, as it stimulates the proliferation and maturation of different types of defense cell. In his laboratory at LNBio, Bajgelman developed two other melanoma lines that secreted immunomodulatory substances such as 4-1BB ligand and OX40 ligand.
Genetic modification was obtained with the aid of recombinant viruses, which infected the tumor cells and introduced into them the gene that encodes the immunomodulator. Once established, the modified cell lines were exposed to radiation.
“When we irradiated the modified tumor cells, they lost the capacity to generate tumors but continued to stimulate the immune system,” Bajgelman said.
The therapeutic strategy consists of making the T cells – lymphocytes that coordinate the immune system’s response to tumors – see cancer cells as enemies to be combated.
According to Bajgelman, findings in the scientific literature show that individuals with cancer typically display high levels of regulatory T cells (Tregs), a type of lymphocyte that inhibits the proliferation of other types that attack tumor cells.
In a physiological context, Tregs have the important mission of keeping the immune system balanced so that the organism’s tissues are not attacked unnecessarily, but in people with cancer, according to Bajgelman, they may protect the tumor.
“The 4-1BB and OX40 ligands interact with receptors on the surface of T cells to boost their activation,” he said. “Our strategy was to produce vaccines that secrete these ligands and combine [them] with GVAX, which secretes GM-CSF.”
The combination stimulates two stages of the anti-tumor immune cycle, he explained: it activates dendritic cells, which process antigen material and present it on the cell surface to the T cells of the immune system, and it co-stimulates T cells to stop them from assuming the immunosuppressant phenotype.
First tests
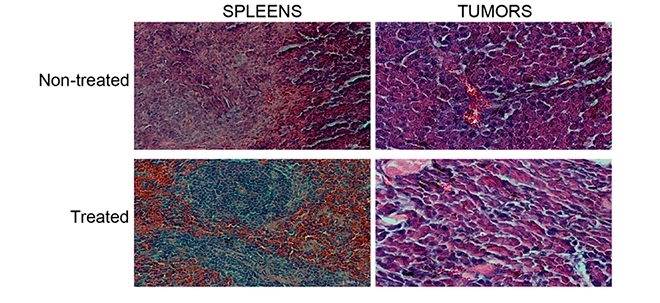
Various combinations of the three modified tumor cell lines were tested at LNBio in experiments with mice. Tumors were induced by injecting melanoma cells subcutaneously into the right flank.
“About two days after inducing the tumor, we began treatment with the vaccines. We applied three doses at two-day intervals,” Bajgelman said.
“We tested each of the three cell lines separately. They all reduced tumor growth compared with the control animals [which received only unmodified tumor cells]. In a second assay, we tested combinations of two lines, and the tumors grew much less than with monotherapy. In some cases, the tumor was totally suppressed.”
In vitro assays with all three modified cell lines in a single treatment produced good results, but the cells did not perform as expected in animals.
“Separate tests of these immunomodulators had previously been described in the scientific literature. We were the first to test different combinations of immunomodulatory lines,” Bajgelman noted.
In another experiment, the mice treated with vaccine combinations that prevented tumor growth were challenged again 30 days later, this time by administering a new injection of unmodified tumor cells with the potential to form tumors.
“The animals that did not develop tumors in the first protocol didn’t do so after this second challenge either. Apparently, the organism created an immunological memory and eliminated the cells as soon as they were injected. The mice were monitored for over a year and failed to manifest the disease,” Bajgelman said.
This kind of strategy, he added, could be used in synergy with other treatments, such as surgical tumor removal and chemotherapy.
“It isn’t unusual for some tumor cells to survive in the organism after conventional treatment. Immunotherapy could protect the patient against relapse,” he explained.
The results of the tests with mice are described in an article published in the journal Frontiers of Immunology.
The LNBio group now plans to create modified tumor cell lines from human cells and begin the first in vitro assays.
“To do this, we’re producing recombinant viruses with human genes. The idea is to use the same immunomodulators as those we tested in mice,” Bajgelman said.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





