

Markers of infection found in blood of patients enabled Brazilian researchers to elucidate cellular signaling pathway involved in both defenses against this virus and formation of new neurons (the figure shows cellular signaling of metabolic alterations caused by Zika virus infection / Frontiers in Microbiology)
Markers of infection found in blood of patients enabled Brazilian researchers to elucidate cellular signaling pathway involved in both defenses against this virus and formation of new neurons.
Markers of infection found in blood of patients enabled Brazilian researchers to elucidate cellular signaling pathway involved in both defenses against this virus and formation of new neurons.
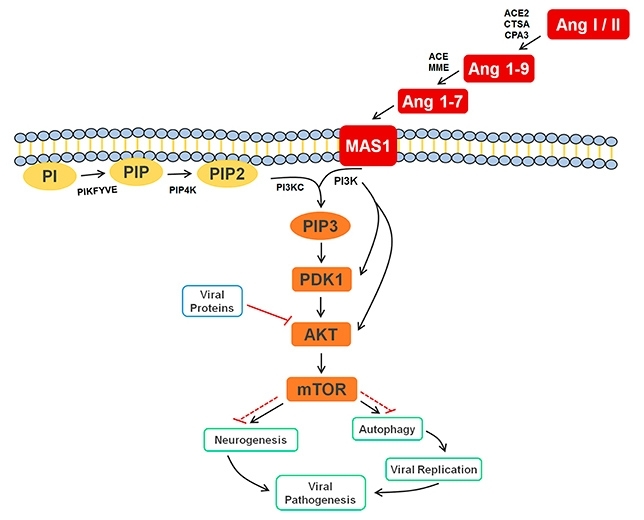
Markers of infection found in blood of patients enabled Brazilian researchers to elucidate cellular signaling pathway involved in both defenses against this virus and formation of new neurons (the figure shows cellular signaling of metabolic alterations caused by Zika virus infection / Frontiers in Microbiology)
By Karina Toledo | Agência FAPESP – Researchers at the University of Campinas (UNICAMP) in São Paulo State, Brazil, have identified molecules that serve as markers of Zika in blood serum taken from patients with this viral infection.
The finding enabled the group to discover an important cellular signaling pathway involved in the immune response to Zika. The study was published in October 2017 in the journal Frontiers in Microbiology.
“This same cellular signaling pathway is involved in neurogenesis – the process of new neuron formation – and is very active during development of the embryo. We know some viruses, including Zika, release a protein that blocks this signaling cascade in order to escape the immune system, and this may also be associated with microcephaly and other central nervous system malformations,” said Carlos Fernando Melo, first author of the article.
Altogether, the study involved 79 participants, 35 of whom had a confirmed diagnosis of Zika after testing positive in a molecular methodology that detects viral RNA in blood samples during the acute stage of infection.
Thirty-four other patients included in the study displayed symptoms similar to those caused by Zika, such as fever, conjunctivitis and headache, when the material was collected for analysis but tested negative for this virus as well as for dengue and chikungunya. A third group comprised ten healthy individuals who had no symptoms of infection.
Samples were collected and analyzed as part of Melo’s PhD research, with FAPESP’s support and supervision by Rodrigo Ramos Catharino, a professor in UNICAMP’s School of Pharmaceutical Sciences (FCF) and head of its Innovare Biomarker Laboratory.
“We sorted the samples into two groups. One contained only cases that tested positive for Zika. The other, considered the control group, contained material from both symptomatic patients who tested negative and healthy volunteers. We did this precisely to avoid markers not specific to Zika that could be associated with infections caused by other pathogens,” Melo explained.
Blood serum from the participants was analyzed in a mass spectrometer, a device that enables scientists to identify the compounds present in a sample by measuring the mass of their molecules. The results were interpreted using a statistical model known as orthogonal partial least squares discriminant analysis (OPLS-DA).
“This methodology enabled us to rank differences between samples by order of importance and hence to identify the metabolites that differentiated the two groups,” Melo said. “We were surprised to find that the samples from infected patients contained the peptides angiotensin 1-7 and angiotensin I, which are part of the renin-angiotensin system.”
He explained that the peptides, enzymes and cellular receptors that form the renin-angiotensin system are associated mainly with the control of blood pressure and body fluid volume. However, recent studies have shown that some elements of this system play a key role in the immune response against viruses.
As reported by the authors in the article, experiments performed by other groups showed that rats infected with dengue virus and treated with losartan or enalapril presented more severe symptoms of viral infection. These two drugs act against hypertension by inhibiting angiotensin-converting enzyme (ACE), which converts the hormone angiotensin I to the active vasoconstrictor angiotensin II.
In another experiment, rats genetically modified so as not to express ACE were infected with respiratory syncytial virus and later presented a viral load five times higher than that in wild-type rats (capable of expressing ACE).
“Data from the scientific literature suggests that in the case of Zika, the peptides angiotensin 1-7 and angiotensin I are involved in the cellular immune response. Apparently, they give the signal for the start of autophagy [in which the structures of the intracellular medium are broken down], so as to prevent replication of the virus, but this is a hypothesis that needs to be confirmed,” Melo said.
The scientists also found that the positive samples contained a group of lipidic mediators that are part of the signaling cascade initiated by angiotensin when it bonds to its cellular receptor. According to Melo, this finding confirmed participation by these peptides from the renin-angiotensin system in the immune response against Zika.
One starting point, two outcomes
The signaling pathway that theoretically leads cells infected by the virus to self-destruct in order to halt the infection is mediated by a protein known as the mammalian target of rapamycin (mTOR). Under certain circumstances, this protein can regulate the onset of neurogenesis. The factors that determine whether signaling will go one way or the other are poorly understood.
“We know neurogenesis is much less active in adults than in developing embryos. We now plan to study the mTOR pathway in greater detail in order to understand when and how signaling leads to autophagy or neurogenesis,” Melo said.
This knowledge could pave the way for the development of therapies that block infection by Zika before the virus causes damage to the central nervous system, he added.
Another future possibility would be to use markers found in blood to help clinicians with diagnosis. “We could use the same approach with different technological tools to obtain a set of markers that distinguish positive cases, but to do so, we need partners in information technology and data processing, as well as financial support to continue the research,” said Diogo de Oliveira, a postdoctoral fellow at UNICAMP and a co-author of the article.
According to Catharino, the study presents the most complete physiopathological description of infection by Zika in humans to date. “Thanks to the tools of metabolomics, we succeeded in identifying unusual markers of infection [peptides and lipids instead of proteins and DNA] both quickly and directly, without needing models or cell culture. This is a highly applicable but entirely novel approach,” he said.
The study was only possible thanks to collaboration with researchers from the Zika-UNICAMP Network. “We’re working with the Network to develop a diagnostic method for two kinds of biological fluid,” Catharino said. “We need partners and funding to continue.”
The article “Serum metabolic alterations upon Zika infection” can be read at: frontiersin.org/articles/10.3389/fmicb.2017.01954/full.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





