

Researchers proposed this hypothesis at a Brazilian university on the basis of a review of articles published after the 2015 surge in cases of microcephaly in Brazil (photo: Wikimedia Commons)
Researchers proposed this hypothesis at a Brazilian university on the basis of a review of articles published after the 2015 surge in cases of microcephaly in Brazil.
Researchers proposed this hypothesis at a Brazilian university on the basis of a review of articles published after the 2015 surge in cases of microcephaly in Brazil.
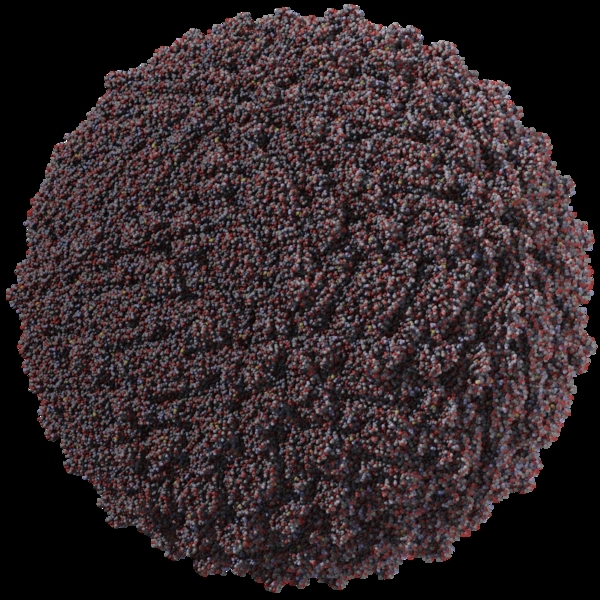
Researchers proposed this hypothesis at a Brazilian university on the basis of a review of articles published after the 2015 surge in cases of microcephaly in Brazil (photo: Wikimedia Commons)
By Karina Toledo | Agência FAPESP – Recent studies have confirmed that congenital infection with the Zika virus, especially in the first trimester of pregnancy, can result in severe damage to the newborn’s brain, the most frequently occuring of which is microcephaly. However, the mechanisms leading to malformation of the central nervous system are not yet clear.
New hypotheses have been presented by researchers at the Federal University of the ABC (UFABC) in São Paulo, Brazil. In an article published in Molecular Neurobiology, the authors report that the currently available scientific evidence suggests that infection with Zika impairs interactions between neurons and glial cells. These interactions are considered essential to the development of the cerebral cortex, the outermost layered structure of the brain.
The study was conducted during Laís Takata Walter’s PhD research, with FAPESP’s support and supervision by Alexandre Hiroaki Kihara, a professor at UFABC’s Center for Mathematics, Computation & Cognition (CMCC).
The researchers collated and reviewed many of the articles published on the effects of Zika since the 2015 surge in cases of microcephaly and correlated their findings with existing knowledge of neurodevelopmental processes.
Márcia Aparecida Sperança, a professor at UFABC’s Center for Natural & Human Sciences (CCNH), collaborated with Kihara on the study, as did researchers at the University of São Paulo (USP) in Brazil and the University of Reading in the United Kingdom.
“There are studies that suggest that Zika infection modifies the expression of genes that code for connexins, a family of gap junction proteins responsible for, among other things, promoting interconnections between neurons and glial cells. But the consequences of this fact for brain development aren’t explored in these articles,” Kihara said.
Glial cells can be divided according to their form and function into oligodendrocytes, astrocytes, Schwann cells, ependymal cells, and microglia. The central nervous system is estimated to contain approximately ten glial cells for every neuron, but glial cells are so small that they account for only half the volume of nervous tissue in the body.
According to Kihara, most cortical neurons originate in the ventricular zone, the lining of the brain ventricles, which contains vast numbers of neural stem cells. The differentiation of neurons takes place largely during the process of migration to the cortex, and the glial cells act as guides to ensure that they follow the correct path.
“Neurons and glial cells must be coupled for migration to occur,” Kihara said. “Our hypothesis is that any alteration in connexin expression makes the process less efficient. Indeed, there are studies that show a smaller number of cortical neurons in babies exposed to Zika during pregnancy.”
As another outcome of their review of the scientific literature, the researchers at UFABC suggest that congenital infection with Zika promotes a combination of two different cell death pathways: apoptosis (programmed cell death) and autophagy (intracellular self-degradation of external structures).
“During the development of the central nervous system, both cell proliferation and cell death occur naturally,” Kihara said. “Apoptosis is a controlled death mechanism whereby the tissue sculpts itself. Some studies suggest that Zika infection deregulates the expression of genes associated with both apoptosis and autophagy, but exactly how this affects the nervous tissue needs to be investigated.”
New lines of research
For approximately a decade, Kihara’s group has studied the role of connexin-encoding genes in various models of diseases that affect the central nervous system, such as epilepsy and cerebral palsy.
“Now we’ve begun studying the same thing in the context of Zika infection,” Kihara said.
In an interview with Agência FAPESP, Walter explained that the original aim of her PhD research was to investigate details of retinal development and that she became interested in Zika after reading that the infection also causes alterations in the visual system.
“I began reading about Zika out of sheer curiosity, and my interest kept growing,” Walter said. “In this article, we compiled the main findings and also suggested new lines of research.”
In collaboration with Sperança and Kihara, Walter now plans to investigate how Zika infection interferes with neuron migration and the formation of new synapses in animal models.
“Many studies focus on how the virus causes neuronal death,” she said. “We want to find out how the neurons that survive the infection are affected. Does the virus also alter connectivity among them?
The article “Evaluation of possible consequences of Zika virus infection in the developing nervous system” can be retrieved from link.springer.com/article/10.1007%2Fs12035-017-0442-5.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





