
Inoculation developed by researchers in Brazil proves safe and induces production of antibodies against Streptococcus pyogenes bacteria in animal trials
Inoculation developed by researchers proves safe and induces production of antibodies against Streptococcus pyogenes bacteria in animal trials.
Inoculation developed by researchers proves safe and induces production of antibodies against Streptococcus pyogenes bacteria in animal trials.
Inoculation developed by researchers in Brazil proves safe and induces production of antibodies against Streptococcus pyogenes bacteria in animal trials
By Karina Toledo
Agência FAPESP – The vaccine against rheumatic fever — an inflammatory disease that affects genetically susceptible people after a bacterial infection — should begin to be tested in humans this year by researchers from the Universidade de São Paulo’s Heart Institute (InCor).
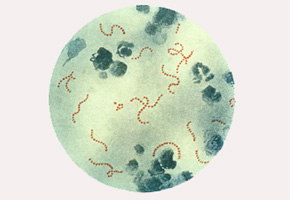
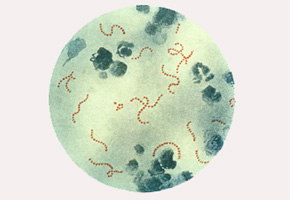
Experiments conducted in rodents and small pigs suggest that the vaccine is safe and induces a specific immune response against Streptococcus pyogenes bacteria.
In most infected individuals, this pathogen causes only a sore throat. In predisposed children, however, contact with S. pyogenes can induce an autoimmune disease. In an attempt to defend itself from the bacteria, the immune system begins to attack its own tissue, and the heart is the main target.
“This happens because parts of the bacteria have amino acid sequences and protein conformations that are very similar to those in cardiac valves,” explained Luiza Guilherme, a researcher at InCor and the coordinator of the study.
The disease can also cause pain in joints, known as polyarthritis, which normally improves over time. However, the damage to cardiac valves is progressive and permanent, eventually leading to a need for corrective surgery.
“When the patient is operated on for the first time as a child, the chance of needing several surgeries over a lifetime is great. For this reason, rheumatic fever is one of the most expensive diseases to treat in Brazil and worldwide,” Guilherme stated.
It is estimated that only 3% or 4% of people are susceptible to developing an autoimmune disease after infection with S. pyogenes. Still, the cost of the treatment of rheumatic fever to the Public Health System (SUS) is behind only AIDS. In 2007, according to the researchers, US$ 30 million was spent to treat the disease, and US$ 60 million was spent on cardiac surgeries. The Health Ministry does not have the latest figures on spending.
At InCor, where there are approximately 600 patients with rheumatic cardiac disease per month, 2,000 patients are on the waiting list for valvular surgery. Nearly 40% of those patients are children.
The quest for a bacterial antigen capable of inducing a protective immune response began in 2000 with the support of FAPESP’s Program for Research Partnership for Technological Innovation (PITE). Currently, research is conducted under the auspices of the Institute of Investigation in Immunology, one of the National Institutes of Science and Technology (INCTs) installed in São Paulo and funded by FAPESP and the National Council of Scientific and Technological Development (CNPq).
“The first step was to define the epitope, or the minimal fragment of bacteria that can induce an immune response. To this end, we analyzed the serum of normal individuals who had contact with bacteria and did not develop autoimmune disease. The idea was to discover which part of the bacteria the individual reacts to,” explained Guilherme.
Within protein M — a molecule secreted from the external wall of the bacteria — the scientists identified a group of 55 amino acid residues that could be recognized by the antibodies and lymphocytes of the human immune system.
“Protein M has a region, ‘A,’ that is constantly mutating. The amino acid residue changes and gives rise to new types of bacteria. There is a region, ‘B,’ that sets off the autoimmune reaction, but there are also ‘C’ and ‘D’ regions, which are equal in practically all strains and do not cause the disease. We identified the sequence of amino acids for the vaccine in region C,” explained the researcher.
A synthetic version of the sequence of amino acids was produced in the laboratory and injected into several mouse models. One of the experiments used a transgenic line of rodents that expressed human leukocyte antigen (HLA) class II molecules, which are directly involved in the identification of antigens and the development of an immune response.
“The idea was to mimic the genetic susceptibility to autoimmune disease found in certain human patients and to evaluate the safety of the vaccine. We followed animals for a year and observed that the immunizer did not induce any type of lesion or alteration in the organs,” explained Guilherme.
To test the vaccine’s protective capacity, scientists submitted mice to an immunological challenge. “The animals were infected with enormous quantities of the bacterium, enough to induce a peritoneal abscess. The immunized group had an 80% survival rate after one month, and the others died the next day,” the researcher commented.
Posterior tests with rodents indicate that the vaccine induced the production of large quantities of specific antibodies against S. pyogenes. The results were published in an article in Vaccine magazine.
Experiments were also undertaken in small pigs weighing approximately 25 kg, similar to a child. The animals were monitored for one year and had high antibody titers and no deleterious reaction.
“With these results in hand, we are ready to begin phase 1 studies in humans. We are only awaiting the release of preapproved financing from the Brazilian Development Bank (BNDES),” explained Guilherme.
At first, only healthy adult volunteers will be vaccinated. The objective is to verify whether the vaccine can induce the production of specific antibodies. “The volunteers will be examined by cardiologists, immunologists and infectologists, and in parallel, we will include a control for autoimmunity. If the results are promising, we can begin trials in children and with a greater number of volunteers,” stated the researcher.
The article, “HLA class II transgenic mice develop a safe and long lasting immune response against StreptInCor, an anti-group A streptococcus vaccine candidate” (doi: 10.1016/j.vaccine.2011.08.113) can be read at www.sciencedirect.com/science/article/pii/S0264410X11013909.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





