

A strategy for treating acute myeloid leukemia is being tested in humans. Preliminary results were presented to the Next Frontiers to Cure Cancer meeting (image: Wikimedia Commons)
A strategy for treating acute myeloid leukemia is being tested in humans. Preliminary results were presented to the Next Frontiers to Cure Cancer meeting.
A strategy for treating acute myeloid leukemia is being tested in humans. Preliminary results were presented to the Next Frontiers to Cure Cancer meeting.
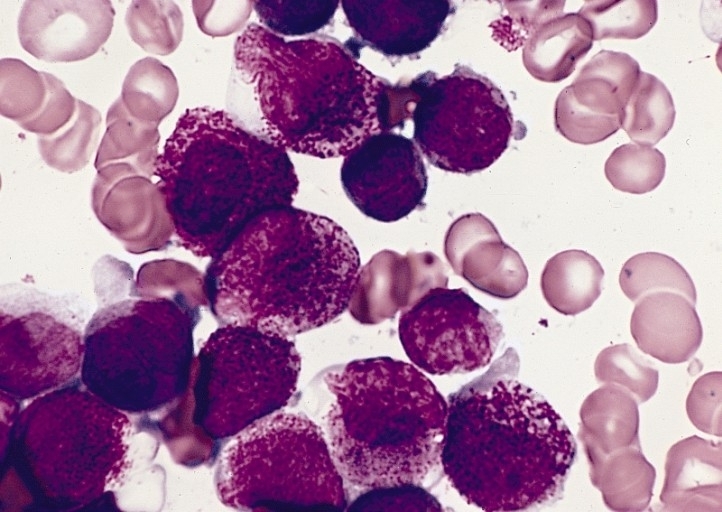
A strategy for treating acute myeloid leukemia is being tested in humans. Preliminary results were presented to the Next Frontiers to Cure Cancer meeting (image: Wikimedia Commons)
By Karina Toledo | Agência FAPESP – Reprogramming tumor cells to make them produce a substance that stimulates the immune system to combat cancer is the strategy underlying a new treatment against leukemia that is being tested in humans in Canada.
Phase I clinical trials, which aim to prove that the method is safe, are under way at the Princess Margaret Cancer Center in Toronto, led by immunologist Christopher Paige. The PM Cancer Center is part of the University Health Network (UHN).
Recent results were presented on April 20, 2017, during a conference entitled Next Frontiers to Cure Cancer, organized in São Paulo, Brazil, by A.C. Camargo Cancer Center.
“We’re testing this approach in the treatment of acute myeloid leukemia (AML), a type of cancer that starts in the bone marrow, making it produce abnormal white blood cells. If it works, the same principle could be used against any kind of tumor with the potential to cause metastasis,” Paige said in an interview given to Agência FAPESP.
The technique consists of removing tumor cells from the patient, reprogramming these cells in vitro using a viral vector, and injecting them back into the patient in a single dose. The goal is to make the modified malignant cells express the protein interleukin-12 (IL-12), a pro-inflammatory cytokine that is capable of stimulating the immune system to combat the disease.
“To be able to grow and spread through the organism, tumors have to be capable of neutralizing the immune system’s radars. Malignant cells often secrete substances that make the defense cells become tolerant of the foreign body. IL-12 can reverse this tolerance profile,” Paige explained.
The pro-inflammatory cytokine acts at different levels, Paige continued. It can activate defense cells known as helper T cells, or CD4+ T lymphocytes, which secrete large amounts of another cytokine called interferon gamma (IFN-γ). This in turn boosts the activity of other defense cells, such as macrophages.
IL-12 can also activate a type of lymphocyte called natural killer (NK) cells, which have an important role in the fight against tumor cells. NK cells assist in the maturation of cytotoxic T cells, or CD8+ lymphocytes, which directly attack cells foreign to the organism by producing enzymes.
“Our hypothesis is that when the reprogrammed cells are put back in the patient, they will spread through the organism until they reach the lymphoid organs [where lymphocytes form and mature, such as the bone marrow, thymus, lymph nodes and spleen]. There, they will activate the immune system, which will attack both our reprogrammed cells and the other leukemic cells. That’s the plan,” Paige said.
The strategy proved safe and effective in preclinical trials in mice. It not only eliminated the disease but also enabled the mice to live as long as healthy rodents – about two years.
So far, only one person has received the treatment. A small number of reprogrammed cells were applied to see whether they triggered an immune response and, if so, which defense cells were recruited. Another aim was to measure the levels of pro-inflammatory substances released.
“We’re going to keep track of this patient for 30 days, long enough to be sure we’re not doing any harm to the patient. At the end of that period, if all goes well, we’ll treat a second patient. And so we’ll go on, treating one per month until we reach ten. We’ll take at least a year to be sure it’s safe and to get a clearer idea of how the method works in humans,” Paige said.
The main risk, he added, is that an excessive amount of IL-12 in the body could unleash a storm of inflammatory cytokines, which could impair organ function and even lead to death. In preclinical trials, however, no severe adverse effects were observed.
Target population
Acute myeloid leukemia is characterized by the rapid proliferation of abnormal white cells, which do not mature, do not perform their function and which build up in the bone marrow, interfering with the production of red blood cells and platelets.
Symptoms vary considerably but may include bone pain, weight loss, enlarged lymph nodes, anemia, recurring infections, bruising and bleeding. AML represents 25% of leukemia cases in adults and has the lowest survival rate of all leukemia types.
The disease usually spreads swiftly and can affect the lymph nodes, liver, spleen, brain, bone marrow and testicles. The main currently available treatment is chemotherapy, which can lead to total remission in most cases, but according to Paige, over 70% of patients relapse within a year.
“Our original aim was to test the treatment on the patients showing signs of relapse after achieving complete remission,” Paige said. “It would be an option to be tested before going for a bone marrow or hematopoietic stem cell transplant, a procedure considered more toxic and riskier. We thought we’d have time for the tests until a compatible donor was found, but because of changes in Canadian clinical practice, this is happening very quickly. So we had to change our inclusion criteria.”
Patients who have had a transplant and displayed signs of relapse are now being included in the study, according to Paige. There are few therapeutic options for these cases, and most involve experimental drugs.
“Previous studies have tried and failed to stimulate the immune system to combat the cancer using IL-12,” Paige said. “Researchers tried injecting the cytokine directly into the tumor, inserting it into dendritic cells [which capture foreign antigens and present them to lymphocytes] and tumor-infiltrating lymphocytes, or TILs.”
For Paige, the advantage of the new approach is that it helps to spread IL-12-producing cells to different lymphoid organs. “We don’t yet know where is the best place to induce immunity against cancer, but IL-12-producing cells will spread everywhere,” he said. “Also, the immune system can adapt if the tumor undergoes mutations, which decreases the likelihood of resistance to the treatment.”
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





