

Researchers at Redoxome performed experiments to understand the mechanisms involved in the chemical reactions that produce free radicals (image: SP Pesquisa)
Understanding how these substances act in blood vessels is the aim of a group of scientists affiliated with Redoxome, a research center supported by FAPESP.
Understanding how these substances act in blood vessels is the aim of a group of scientists affiliated with Redoxome, a research center supported by FAPESP.
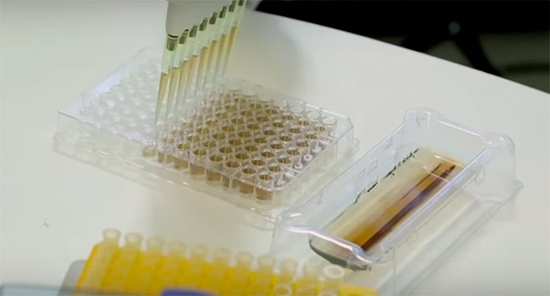
Researchers at Redoxome performed experiments to understand the mechanisms involved in the chemical reactions that produce free radicals (image: SP Pesquisa)
By Karina Toledo
Agência FAPESP – The benefits of antioxidants for the cardiovascular system have been described many times in the scientific literature. Understanding the mechanisms of their action is one of the aims of a group of researchers coordinated by Dr. Francisco Laurindo, a professor at the University of São Paulo’s Heart Institute (INCOR-USP) in Brazil.
The work is being done at the Center for Research on Redox Processes in Biomedicine (Redoxome), one of FAPESP’s Research, Innovation and Dissemination Centers (RIDCs). In one of its research projects, the group is investigating the role played by protein disulfide isomerase (PDI) in remodeling blood vessels and preventing their constriction.
“Remodeling is the most powerful mechanism for controlling the blood vessel lumen, the inner cavity through which blood flows,” Laurindo explained. “It can be physiological, caused by a reduction in demand, as occurs in a woman’s abdominal aorta after she gives birth, or it can be pathological remodeling due to an arterial lesion, for example, which causes the artery to constrict and hampers circulation.”
The best-known role of PDI, according to Laurindo, consists of helping the proteins produced in the endoplasmic reticulum to mature into a functional form. It does this by oxidizing certain amino acids.
However, Redoxome’s studies are showing that PDI is also important, among other things, to avoid pathological arterial constriction after a lesion caused by a procedure like angiography, in which a catheter is inserted into a blood vessel.
“When your skin is grazed or cut, the fibroblasts secrete collagen fibers that bind up the damaged tissue, which heals by constriction. That’s why a scar has that puckered look. Most types of tissue heal like this, but blood vessels would become blocked if they healed in exactly the same way. We suspect PDI participates in the mechanism that keeps blood vessels open during the healing process,” Laurindo said.
To test their hypothesis, the researchers induced a femoral artery lesion in rabbits using a catheter with an inflatable balloon at its tip. After 14 days, they observed a significant increase in PDI expression at the site.
The researchers repeated the experiment, but this time, they reopened the femoral artery on the twelfth day for treatment with a special gel containing an antibody capable of neutralizing the action of PDI.
“We used pluronic gel, which has a curious property: it becomes liquid at or around zero degrees Celsius and solidifies at body temperature. We placed the gel in a refrigerator, mixed it with antibodies, and applied a layer around the artery. The solidified gel then began releasing antibodies and continued doing so for the next two days,” Laurindo said.
Caliber loss in the artery treated with anti-PDI reached about 40% after two days of treatment, evidencing intense constrictive remodeling. In a control artery in the same animals, treated only with gel and a placebo after the lesion was induced, lumen reduction reached only 10% in the same period.
“After lesion formation, the cytoskeletons of blood vessel wall cells are completely restructured. PDI participates in this process, and we’ve identified a possible target: a molecule called beta-1 integrin. It’s found on the surface of blood vessels and helps convey signals for the organization of cell cytoskeletons,” Laurindo said.
However, in his view, it is still too soon to say that beta-1 integrin will definitely be a target worth exploring for the treatment of diseases like atherosclerosis.
“It’s possible that treatment with a substance capable of mimicking PDI may help keep the blood vessel open after a lesion,” he said. “We tried doing this with rabbits but observed no such effect. However, our experiment was performed on healthy arteries. Now, we must test the treatment in a model that mimics human atherosclerosis.”
Not always beneficial
While advancing their knowledge of PDI’s role in blood vessels, the researchers were surprised when another study produced findings that contradict the belief that lipoic acid, a powerful antioxidant, can help to prevent cardiovascular disease.
Preliminary data suggest that regular intake of lipoic acid may be harmful to patients with Marfan syndrome, a genetic disorder that affects connective tissue and can cause dilation and rupture of the aorta.
“Alpha-lipoic acid is widely sold all over the world as a dietary supplement and is considered pretty safe. We were surprised by the negative result of treatment in mice,” Laurindo said.
The experiment was performed in rodents that had been genetically modified so that they developed a condition similar to Marfan syndrome. The animal model was designed by geneticist Lygia da Veiga Pereira and her team. Pereira is a professor at the University of São Paulo’s Bioscience Institute (IB-USP).
Marfan syndrome can be caused by various mutations, both inherited and sporadic, in the gene for fibrillin-1 protein and is estimated to affect one in every 10,000 newborns.
The main manifestations of the disease include abnormal bone growth, chest deformities, eyesight problems, heart valve prolapse and aortic aneurysm, or dilation of a segment of the artery that can lead to its rupture and cause death.
“The aorta is essentially an elastic tube, and fibrillin is the key component of its elastic microfibrils. Protein deficiency in Marfan syndrome reduces aortic resistance, and as a result, the aorta tends to dilate when blood is pumped out of the heart,” Laurindo explained.
In previous experiments, the group at INCOR-USP had observed increased production of oxidizing substances, such as hydrogen peroxide and superoxide radicals, by the aorta of mice with Marfan syndrome in their sixth month, when the disease is at an advanced stage.
These molecules are traditionally considered harmful to cells because they can damage proteins, lipids and other components that are important to cell functioning. “We treated a group of rodents with losartan, an antihypertensive drug, and observed that the medication improves the phenotype of the disease considerably, as described in the scientific literature. Six-month-old mice treated from birth had a much less dilated aorta than mice that received a placebo. We then decided to find out whether the use of lipoic acid could reproduce the same therapeutic effect as for losartan. What we observed was the opposite,” Laurindo said.
The researchers compared three groups of mice with Marfan syndrome. The control group was treated solely with placebo. The second group received only losartan, and the third was given lipoic acid. Treatment began 21 days after birth and lasted until the mice were between one and six months old.
Histological analysis of the aorta was performed, as well as echocardiography (ECG). Optical coherence tomography (OCT) was also conducted at six months. “We showed by two different methods that the production of oxidizing substances was in fact reduced in the group that received lipoic acid. However, the aortic aneurysm occurring in the sixth month was even worse than in the control group,” Laurindo said.
The scientists found more severe damage to elastic fibers in the aorta of the mice treated with antioxidant supplement, resulting in an increase in collagen synthesis, which is a process known as fibrosis. This aggravated the loss of aortic function, making the aorta expand even more than in the placebo-treated mice. “Aneurysm appears to be an exception among cardiovascular diseases,” Laurindo said. “The results of this study suggest that oxidizing substances play a protective role, at least in the advanced stage of the disease. We now plan to study the mechanisms involved in this process in more detail.”
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





