

Only 60% of patients respond to treatment with conventional antidepressants (detail of Vincent van Gogh’s painting Sorrowing Old Man/Wikimedia Commons)
Whereas conventional drugs require prolonged treatment to be effective, compounds that inhibit an enzyme involved in DNA methylation have been shown to have antidepressant effects in animals.
Whereas conventional drugs require prolonged treatment to be effective, compounds that inhibit an enzyme involved in DNA methylation have been shown to have antidepressant effects in animals.
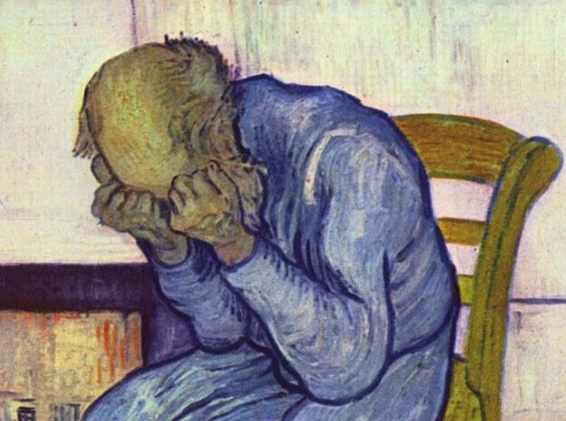
Only 60% of patients respond to treatment with conventional antidepressants (detail of Vincent van Gogh’s painting Sorrowing Old Man/Wikimedia Commons)
By Karina Toledo, in Rio de Janeiro
Agência FAPESP – Situations of prolonged stress and repeated experiences of anger, fear or anxiety can lead to structural and functional changes in the brain that predispose an individual to the development of diseases such as depression.
Conventional antidepressants are capable of reversing these changes in the brain but take at least a fortnight to start having an effect. Moreover, only 60% of patients respond to treatment, and full remission of symptoms occurs in only half of them.
In search of therapies that are more effective and faster acting, researchers at the University of São Paulo’s Ribeirão Preto Pharmaceutical Science School (FCFRP-USP) in Brazil are using animal models to test new classes of drugs designed to inhibit the enzyme DNA methyltransferase (DNMT), which catalyzes DNA methylation, a chemical reaction that adds methyl groups to DNA.
DNA methylation is considered an epigenetic change, i.e., an alteration in the functioning of the genome without a change in the genetic code. It can be induced by means of different biological and environmental stimuli, including stress, which silence certain genes and consequently reduce the expression of proteins.
Recent results from the project, which is supported by FAPESP, were published this year in the journal Acta Neuropsychiatrica and presented by researcher Sâmia Joca during the Ninth World Congress of the International Brain Research Organization (IBRO 2015), held in Rio de Janeiro on July 7-11.
“Experiments with mice have shown that several different classes of DNMT inhibitor drugs have antidepressant-like effects. When we combined these inhibitors with conventional antidepressants, also from various pharmacological classes, we observed a synergistic effect between the compounds,” Joca told Agência FAPESP.
Both conventional antidepressants and DNMT inhibitors appear to favor the expression of genes that play important roles in stress resilience, she explained. The difference is that DNMT inhibitors induce this effect more quickly, judging from the results of the experiments performed in Ribeirão Preto.
“When you’re exposed to a stressful situation, your organism releases a series of endogenous mediators, such as glutamate and cortisol, that activate stress-response circuits,” Joca said. “If the release of these mediators becomes chronic and excessive, it can lead to neuronal atrophy or death, impairing the functioning of brain circuits that regulate mood, emotions and cognition.”
Evidence in the scientific literature suggests that stress also reduces synapse formation, neurogenesis and cell proliferation in certain parts of the brain, all of which jeopardize neuroplasticity (the brain’s ability to change to adapt to environmental stimuli).
There are proteins that protect neurons from the damage caused by stress. The best known of these is brain-derived neurotrophic factor (BDNF). “However, evidence suggests stress-induced DNA methylation makes chromatin more condensed in cell nuclei and thereby hinders BDNF gene expression,” Joca said. “It may also inhibit other factors that are important to neuron survival. We believe this impairment of neuroplasticity, which is important to maintain stress resilience, may lead in the long run to a predisposition to develop mental health disorders.”
Studies by other groups, she explained, have already shown that one of the effects of chronic treatment with conventional antidepressants is an increase in BDNF expression, especially in the cortex and hippocampus, the brain regions most affected by stress. They have also shown that antidepressants have no effect if BDNF expression is blocked.
“In our view, by boosting the release of neurotransmitters such as serotonin or noradrenaline conventional antidepressants trigger a cascade of intracellular effects that ultimately interfere with DNA methylation levels,” Joca said. “But because this is an indirect effect, chronic treatment is required for it to appear. So we imagined that drugs capable of interfering directly with DNA methylation might have an acute antidepressant effect.”
To test this hypothesis, the Ribeirão Preto group performed a type of experiment used for more than 30 years to screen the effects of antidepressant candidate drugs in mice and rats. Known as the forced swimming test (FST), the model consists of placing the animals for 15 minutes in a water tank from which they cannot escape, however hard they try. On the next day, the test is repeated for five minutes.
“Unlike other classes of central-acting drugs, antidepressants in general make the animals keep swimming to try to escape for a longer time on the second day of the experiment,” Joca said. It’s as if the drug stops them from giving up easily. So if this effect is observed in the FST in response to a new treatment, it’s considered predictive of antidepressant potential.”
Using this acute stress model, the group tested two different DNMT inhibitors: an experimental drug known as RG108 and decitabine, a drug already in clinical use as a chemotherapeutic agent.
The first results of the experiments using only decitabine were published in 2012 in the British Journal of Pharmacology.
“Both decitabine and RG108 interfere with DNA methylation but via completely different mechanisms, and in this acute stress model both had the same effect as the conventional antidepressants fluoxetine and desipramine, but more rapidly,” Joca said.
In a new experiment, the group combined all four drug classes (fluoxetine, desipramine, decitabine and RG108) in subeffective doses, i.e., less than the dose required to obtain a therapeutic effect in isolation. A significant antidepressant effect was observed in all combinations.
“If only one or two combinations had worked, it could be something specific to a particular drug,” Joca said. “But given that they all had this effect, there are appears to be synergy between DNMT inhibitors and conventional antidepressants. The combined effect is greater than the sum of their individual effects. This approach would be interesting in the clinical setting: the dose would be smaller than when each drug is used in isolation, so theoretically the adverse side-effects should also be smaller.”
At present, the group’s research is focusing on how DNMT inhibitors alter the level of gene expression in the cortex and hippocampus, especially BDNF expression. They plan to publish the results soon.
“What we’ve found is that DNMT inhibitors don’t reduce DNA methylation in all brain regions, but they do appear to modulate the effect of stress in the brain,” Joca said.
Chronic stress model
After the first positive evidence with decitabine, the group decided to test DNMT inhibitors in a chronic stress model designed to induce similar behavioral and endocrine alterations in rats to those observed in depressed humans.
The model consisted of exposing the rats to 30 sessions of intense stress. After seven days, the animals were placed in the same environment as in the previous test but in conditions that allowed them to control their exposure to stress.
“When we compared the rats subjected to the initial stress sessions with an unstressed group, we found that it was harder for the former to learn to control exposure to stress on the day of the test,” Joca said.
In this model, the researchers noted that treatment with conventional antidepressants took about seven days to alter gene expression in the cortex and affect the animals’ behavior.
The DNMT inhibitors, in contrast, promoted alterations after acute administration. A single injection administered after the first day of stress was sufficient to induce an antidepressant-like effect (evidenced by an attenuation of the effects of pre-exposure to stress) and make both the level of methylation in the cortex and the animals’ behavior more similar to those of the unstressed group.
However, Joca explained, the idea at this time is not to propose the use of DNMT inhibitors as a clinical treatment for depression, but to understand the intracellular mechanisms induced by these compounds and produce knowledge about pathways that could be explored pharmacologically.
“The risk-benefit ratio of using decitabine could be evaluated in the case of a severely depressed patient at risk of suicide, since the drug has already been approved for use in humans,” Joca said.
Cases of this type have been treated with ketamine, a drug approved for use in humans as a local anesthetic and that has also been shown to have acute and sustained antidepressant effects, with a single dose lasting up to two weeks.
“Studies in the literature describe how ketamine regulates the expression of several genes,” Joca said. “We’re investigating to discover the mechanism whereby it induces this acute antidepressant effect. The problem is that ketamine is a drug of abuse, and the patient risks becoming dependent or suffering an overdose. So we need to find new options with a similar action and less risk of dependence.”
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





