

In an article published in Nature Communications, researchers describe a cascade of events that unbalances the immune system, increasing the risk of recurring infections and death (image: pixabay.com)
In an article published in Nature Communications, researchers describe a cascade of events that unbalances the immune system, increasing the risk of recurring infections and death.
In an article published in Nature Communications, researchers describe a cascade of events that unbalances the immune system, increasing the risk of recurring infections and death.
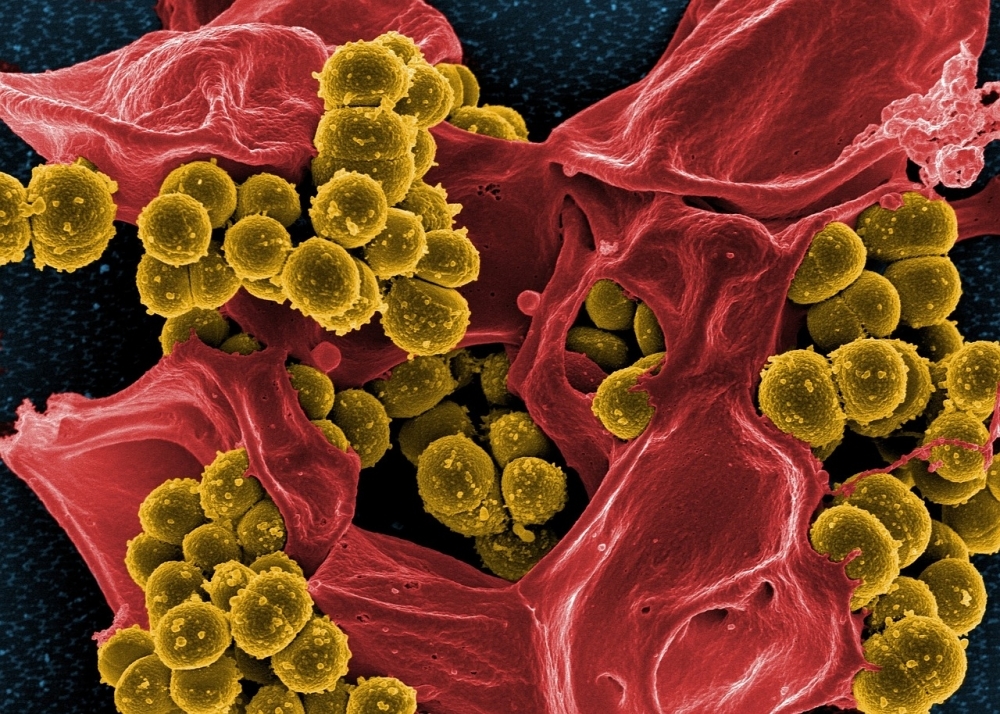
In an article published in Nature Communications, researchers describe a cascade of events that unbalances the immune system, increasing the risk of recurring infections and death (image: pixabay.com)
By Karina Toledo | Agência FAPESP – Patients who survive severe sepsis, which is popularly known as “blood poisoning,” typically experience a sharp fall in immunity in the years following discharge from hospital and become susceptible to cancer and infections with opportunistic pathogens.
The mechanism that causes this immune system dysfunction has now been described in the journal Nature Communications by scientists affiliated with the Center for Research on Inflammatory Diseases (CRID), one of the Research, Innovation & Dissemination Centers (RIDCs) funded by FAPESP. This knowledge could pave the way for developing interventions that mitigate this problem, according to the authors of the article.
“In the most profound stages of sepsis, exacerbated inflammation causes injury to organs such as the lungs, heart, kidneys and liver. Our results show that the mechanism triggered to repair these tissues also eventually leads to immunosuppression,” said José Carlos Farias Alves Filho, a professor at the University of São Paulo’s Ribeirão Preto Medical School (FMRP-USP) and the principal investigator of the study.
He explained that sepsis is a potentially life-threatening systemic inflammation, usually triggered by a localized bacterial infection that has escalated out of control. The condition involves changes in body temperature, arterial blood pressure, heart rate, white blood cell count and breathing. The condition may remain active even after the pathogens have been eliminated. The most critical forms of sepsis involve lesions that can cause vital organs to fail.
“Organ failure can be aggravated by a sharp fall in blood pressure, which hinders tissue irrigation,” Alves Filho said. “This is the worst stage, known as septic shock. Only 50% of patients survive it, and survivors usually suffer neurological, cardiovascular and immunological complications.”
According to data in the scientific literature, the immunosuppression induced by sepsis can last as long as five years, heightening the risk of recurring infections and death.
In a previous study, published in the journal Critical Care Medicine, the research group at CRID showed that 100% of mice that survived severe sepsis died after being exposed to an opportunistic bacterium that causes respiratory infection.
To induce severe sepsis in the mice, the researchers adapted a classic model known as cecal ligation and puncture (CLP), a procedure that involves puncturing the cecum, part of the large intestine, and allowing the feces and intestinal bacteria to spill into the peritoneal cavity. “This procedure leads to the development of peritonitis and simulates what happens in patients with suppurative appendicitis, for example. To induce a more severe condition, we performed four punctures instead of just one, which is the norm, and utilized a thicker needle,” Alves Filho explained.
This model was standardized in the previous study, which showed that after treatment with antibiotics, only 50% of the mice survived. The proportion is similar in humans with severe sepsis.
The immune system of the mice was analyzed 15 days after the acute phase of sepsis ended, and the mice were was found to have over 30% more regulatory T lymphocytes (Tregs), defense cells with immunosuppressive activity.
“Tregs play an important role by preventing the immune system from attacking the organism’s own tissue and triggering autoimmune diseases,” Alves Filho said. “However, these cells must be present in the right proportion. In a healthy organism, they represent between 6% and 10% of all CD4 lymphocytes. Even a small surplus or deficit compromises the maintenance of balance and homeostasis in the immune system.”
Cascade
The more recent study was designed to investigate the factors associated with this observed increase in the population of Tregs in survivors of severe sepsis. To do this, the group used the same experimental mouse model but also analyzed blood samples from 11 patients treated at FMRP-USP’s teaching hospital, Hospital das Clínicas.
“We monitored the patients throughout the acute phase of sepsis,” Alves Filho said. “They were included in the study only after discharge from the hospital. About six to nine months later, we measured blood levels of Tregs and certain cytokines. We found a positive correlation between these levels in mice and in human patients.” Cytokines are signaling molecules that aid cell-to-cell communication in immune responses.
Experiments with animals and with cells cultured in the laboratory enabled the group to map a cascade of events, starting with rising levels of interleukin-33 (IL-33). This is a cytokine that causes the multiplication of M2 macrophages, which secrete several factors that promote tissue repair.
The substances secreted by M2 cells include interleukin-10 (IL-10), a cytokine with anti-inflammatory activity that also promotes the differentiation of naive (immature) lymphocytes into Tregs.
“We observed post-sepsis growth of M2 macrophages in interleukin-10-knockout mice [genetically modified so as not to express IL-10], but not growth of Tregs,” Alves Filho said. “Similarly, when IL-10-knockout macrophages were co-cultured with naive lymphocytes, they didn’t differentiate into Tregs.”
When they analyzed patients’ cells, the researchers found that the levels of IL-10 and IL-33 were twice as high as in people who had never had sepsis. The number of Tregs was also approximately twice as high.
“The study didn’t confirm the origin of IL-33, but we know this substance is secreted mainly by epithelial and endothelial cells. Our hypothesis is that tissue injured by sepsis triggers the entire process,” Alves Filho said.
Next steps
One of the group’s research goals is to find a way to interrupt the cascade of events that leads to the increase in Tregs, without hindering repair of the tissues injured by sepsis. To do this, the researchers are currently investigating the role of adenosine, which augments IL-10 production, in this process.
“We already have data showing a link between growth of M2 cells and changes in levels of adenosine, IL-10 and Tregs. There are also findings that point to a rise in adenosine levels during sepsis. Our hypothesis is that it participates in the process that leads to immunosuppression,” Alves Filho said.
The article “IL-33 contributes to sepsis-induced long-term immunosuppression by expanding the regulatory T cell population” can be read at nature.com/articles/ncomms14919.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





