

Increase in skin elasticity after stem cell transplant, showing success in combating systemic sclerosis (photo: researcher's archive)
Research conducted by a PhD student at University of São Paulo's Ribeirão Preto Medical School in Brazil won four awards in 2016.
Research conducted by a PhD student at University of São Paulo's Ribeirão Preto Medical School in Brazil won four awards in 2016.
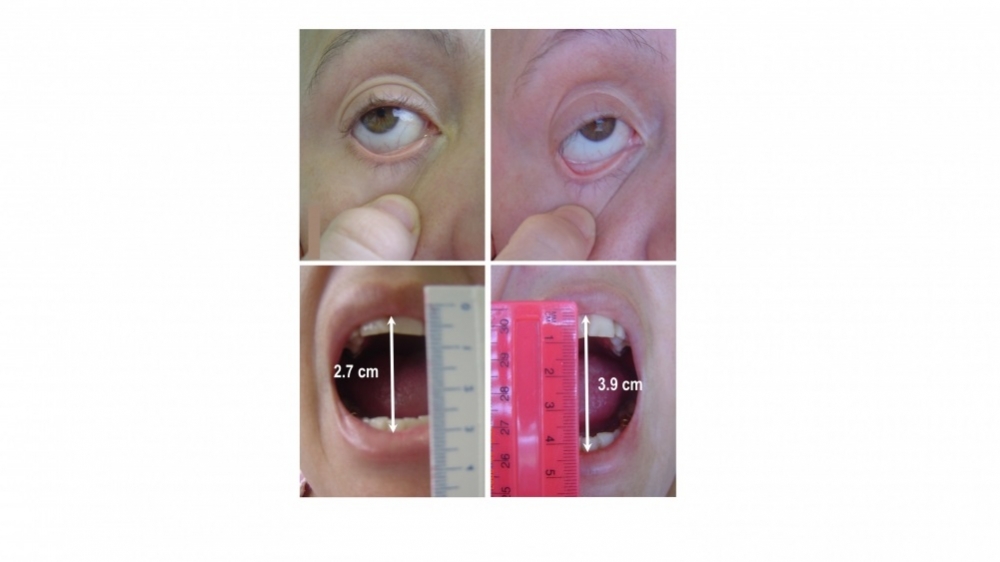
Increase in skin elasticity after stem cell transplant, showing success in combating systemic sclerosis (photo: researcher's archive)
By José Tadeu Arantes | Agência FAPESP – Systemic sclerosis is an autoimmune disease in which the immune system malfunctions and attacks the body’s own connective tissue. The most evident symptom is loss of skin elasticity, causing hardening of the skin. The most severe forms of the disease, however, may result in kidney, lung and heart failure, leading to death.
Conventional treatment with immunosuppressive drugs typically causes adverse side effects and is frequently unsuccessful. Most patients do not respond well, and the mortality rate five years after diagnosis can be as high as 50% in the patient group comprising the most severe cases. As a result, there is a great deal of interest in developing new therapeutic strategies, such as the transplantation of autologous hematopoietic stem cells. Using the vocabulary of information technology, some scientists call this procedure 'resetting', in the sense that the immune system is completely “switched off” and then “switched back on again” with the expectation that it will then work properly.
A study conducted at the University of São Paulo’s Ribeirão Preto Medical School (FMRP-USP) in Brazil investigated how stem cell transplants produce a new immune system and why most, but not all, patients respond well to the procedure. The study was performed by PhD student Lucas Coelho Marlière Arruda, with Professor Maria Carolina de Oliveira Rodrigues supervising and with support from FAPESP under the project “Study of immunological mechanisms involved in the therapeutic response of patients with systemic sclerosis to autologous hematopoietic stem cell transplantation”.
The published study findings have been presented at conferences in Brazil and elsewhere, and the researchers won four awards for this work in 2016: a Posters of Merit award at the FOCIS Annual Meeting (Federation of Clinical Immunology Societies, Boston, USA); first place in the Free Topics Competition at the 33rd Brazilian Rheumatology Conference, SBR (Sociedade Brasileira de Reumatologia, Brasília, Brazil); the Thereza Kipnis Award (the top Latin American immunology award for young researchers), SBI (Sociedade Brasileira de Imunologia, Campos do Jordão, São Paulo State); and an ASH Abstract Achievement Award at the American Society of Hematology Annual Meeting and Exposition (San Diego, USA).
“We evaluated two immune system renewal processes,” Arruda told Agência FAPESP. “One via the thymus, which stimulates the development of T-cells, and the other via the bone marrow, where B-cells are produced. We also set out to understand the various cellular and molecular mechanisms involved in the new production of these immune system cells.”
“The study conducted by Arruda was part of the transplant program for autoimmune diseases at FMRP-USP’s general and teaching hospital, Hospital das Clínicas. We’ve used this alternative strategy to treat some 80 patients. It’s also used in the US and Europe. The clinical procedure was perfectly clear, but we lacked a satisfactory explanation for the immune mechanisms involved, and the aim of the study was to find this explanation,” Rodrigues said.
Before describing the study, the different steps of the treatment need to be explained. Allogeneic transplants using stem cells from a healthy donor are ruled out owing to the risk of graft versus host disease (GvHD), in which the donated stem cells view the recipient’s body as foreign and attack its tissues. Hence, treatment entails an autologous transplant using the patient's own blood-forming stem cells.
The first step consists of mobilizing the stem cells using several medications designed to draw them out from the bone marrow into the bloodstream. In the second step, the cells are identified by their phenotype and collected from a vein by passing the blood through a special machine called a cell separator, in a process similar to dialysis or transfusion. This machine separates and collects the stem cells and returns the rest of the blood to the patient. Sedation is not required. The stem cells are then processed, frozen and stored.
The third step requires far more care. It entails the administration of immunosuppressive substances in very high doses to destroy the patient’s entire immune system. The immunosuppressed patient has to be confined in a carefully isolated environment in which pathogens are completely absent so that there is not the slightest risk of opportunistic infection, which could cause the patient’s death.
In the fourth and last step, the frozen hematopoietic stem cells are thawed and reinfused through a vein into the patient’s bloodstream. They make their way to the bone marrow, where they become reestablished and start making new blood cells and recreating a healthy immune system. Patients who undergo an autologous stem cell transplant are typically hospitalized for about 20 days overall.
“The aim of our study was to understand how the thymus and bone marrow are reactivated, or reset, after the transplant, as well as how this relates to the success or failure of the treatment,” Arruda said. “To do this, we sampled the patients’ peripheral blood and evaluated next-generation molecular markers such as TRECs (T-cell receptor excision circles), which can be used to estimate thymus activity, and KRECs (kappa-deleting recombination excision circles), which provide information about bone marrow activity.”
Thirty-one patients were evaluated before the transplant and then every six months until three years after the procedure. They had all been taking immunosuppressive medication for years, but that conventional treatment had not halted progression of the disease. Twenty-five (more than 80%) responded well to stem cell transplantation and were able to give up the conventional treatment. “In these patients, we found that the thymus began working again and, above all, began producing regulatory T-cells, so called because they regulate the immune system,” Arruda said. “And their bone marrow resumed production of regulatory B-cells, which also regulate the immune system.”
“The study showed that the therapy leads to complete renewal of the immune system and not simple repair,” Rodrigues added. “The fact that the thymus starts working again is proof of that, since the thymus is normally very active in childhood and then becomes inactive once the immune system matures. If it’s reactivated and even grows in size, the immune system has evidently been reconstructed.
“The change in the T-cell repertoire is further evidence. The new cells don’t attack the patient but instead confine their activity to protecting the patient against pathogens, just as they should. A third proof is the significant increase in the number of regulatory T-cells and their increased activity, as these cells are vital to the proper functioning of the immune system. However, the main novelty of Arruda’s study is the finding that B-cells are also renewed.”
In the six patients who did not respond well to the treatment, similar immune responses began but were not sustained. The explanation for these poor responses is that in these cases, the sick cells had not been completely eliminated. Some of them survived the transplant and afterward began multiplying again and attacked the connective tissue. “It’s important to note, however, that even these patients benefited from the new therapy. Before it began, they didn’t respond to conventional treatment, whereas after the transplant they did,” Arruda said.
Systemic sclerosis mainly affects women aged 30-55. It is a multifactorial disease whose causes involve both genetic factors and environmental factors (e.g., lifestyle, work, diet, and use of medications).
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





