

Classification of different stages of infection promotes advances in knowledge about infection dynamics and evolution (image: FMUSP)
Classification of different stages of infection promotes advances in knowledge about infection dynamics and evolution.
Classification of different stages of infection promotes advances in knowledge about infection dynamics and evolution.
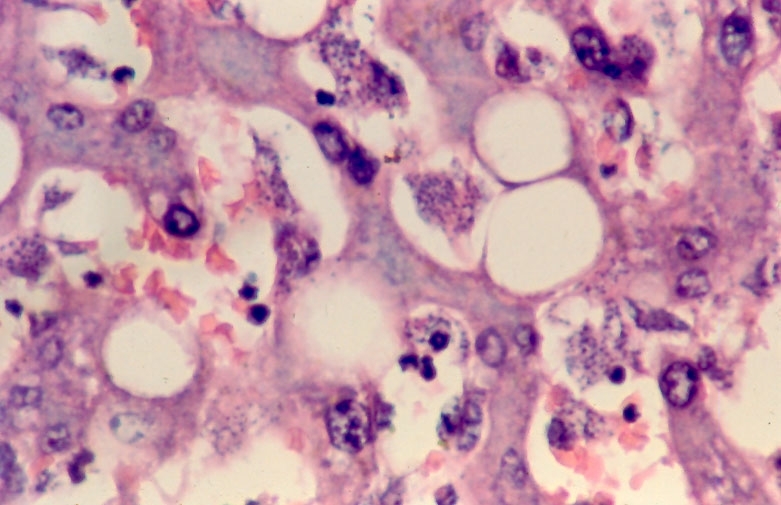
Classification of different stages of infection promotes advances in knowledge about infection dynamics and evolution (image: FMUSP)
By Elton Alisson
Agência FAPESP – After more than 20 years of caring for and monitoring individuals infected by the protozoan Leishmania (L.) infantum chagasi –the agent that causes American Visceral leishmaniasis (AVL)– in areas of the Amazon region that are endemic to the disease, researchers at the Laboratory of Infectious Diseases Pathology of the School of Medicine at the University of São Paulo (FMUSP) and the “Prof. Dr. Ralph Lainson” Leishmaniasis Laboratory of the Evandro Chagas Institute of Belém, Pará State, contemplated some intriguing data.
Of the total number of individuals diagnosed with the infection transmitted by the protozoan, 90% had developed resistance and less than 10% presented symptoms of the disease, which attacks organs such as the spleen and liver and can lead to death if not properly diagnosed and treated.
“Individuals with resistance to the disease remained healthy, despite having established contact with the parasite and presented immunological reactions indicative of infection,” said Carlos Eduardo Pereira Corbett, head of the laboratory and professor in the FMUSP Department of Pathology, in comments to Agência FAPESP.
Curious to know more, researchers from that institution, together with Fernando Silveira, a researcher from the Evandro Chagas Institute, conducted studies revealing that the clinical-immunological profiles of individuals infected with L. (L.) i. chagasi went beyond what was already known by researchers and health professionals.
By identifying immunological markers of the different profiles, the researchers began to gain a deeper understanding of the dynamics of how the infection evolves.
As part of a Thematic Project carried out with FAPESP support, the results of the study were published in the journals Transactions of the Royal Society of Tropical Medicine and Hygiene and Parasitology Research.
“We identified and characterized each of the different clinical and immunological forms of human infection by the protozoan causing American visceral leishmaniasis,” Corbett said. “Based on this classification, we were able to identify which infected individuals evolve towards the resistance side of the spectrum or towards susceptibility for developing the infection,” explained Corbett, who coordinated the study.
According to Corbett, until now, three clinical forms of human infection by L. (L.) i. chagasi had been classified. These were initially identified in the Northeast of Brazil during the 1980s through the use of delayed-type hypersensitivity (DTH) skin tests, which analyze the cellular responses to common antigens on the skin, and ELISA (Enzyme-Linked Immunosorbent Assay) serum tests, which detect immunological disease markers in blood plasma.
Two of the three are symptomatic forms of the infection –the so-called classic AVL and the subclinical oligosymptomatic form– and are presented by fewer than 10% of the infected individuals. The third, however, is a type of asymptomatic infection that manifests in more than 90% of infected individuals.
In the classic symptomatic form, AVL is characterized by fever, a lack of energy (asthenia), weight loss, severe malnutrition (cachexia) and hepatosplenomegaly (enlarged liver and spleen), among other symptoms.
In the oligosymptomatic form, however, patients present with a low-grade or no fever and slightly increased liver and spleen sizes.
In the case of asymptomatic infection, individuals can be serologically positive, and the parasite may have entered their tissues, but the patients display no disease symptoms.
“Although the infected individuals are clinically asymptomatic, from the standpoint of their reaction to the parasite, they are not fully resistant because they were infected in the same way as other patients with symptomatic conditions,” Corbett explained.
New clinical-immunological profiles
In one study of 946 residents from an area endemic to AVL in Pará State, carried out under the FAPESP-funded thematic project, the researchers validated these three clinical-immunological profiles of infection. In addition to these profiles, two new profiles were identified: subclinical resistant infection and indeterminate initial infection.
“It is of fundamental importance that we monitor cases with the indeterminate initial infection clinical-immunological profile to conduct epidemiological surveillance and to allow for early diagnosis of AVL because among these patients are individuals who have genetic conditions that make them susceptible to developing the disease,” Corbett noted.
“These cases are identified by serum positivity for immunoglobulin M (IgM), which is a marker of acute pathogenic infection,” he explained.
According to the researcher, cases of indeterminate initial infection, which do not present the pathogenic immunological marker (IgM), evolve into the subclinical resistant infection profile, as evidenced by a positive Montenegro’s intradermal reaction (MIR)—a reactive test for leishmaniasis that assesses the presence of inflammation or skin rash caused by injecting a solution containing inactive antigens into the skin.
“From the subclinical resistant infection profile, the cases eventually evolve into the resistance profile, which represents the end of the line of the infection for individuals with immunogenetic resistance.”
Delayed hypersensitivity
To characterize the clinical-immunological forms of the infection, the researchers performed MIR tests and indirect fluorescent antibody tests (IFAT), which use a species-specific antigen of L. (L.) i. chagasi to determine the hypersensitivity reaction that indicates the nature of the resistance, to assess the antibody response to the infectious agent in 946 residents of the endemic area.
Of this total, 231 were positively diagnosed with the infection—in other words, they presented reactivity to the MIR test, the IFAT, or both immunological markers of infection. Of the 231 positive diagnoses, 73.2% were classified in the asymptomatic infection profile, 12.1% in the subclinical resistant infection profile, 9.9% in the indeterminate initial infection profile, 2.6% in the symptomatic infection profile, and 2.2% in the oligosymptomatic subclinical infection profile.
By measuring the immune response of the individuals to infection by the protozoan, the researchers determined that resistance is strongly linked to the delayed-type hypersensitivity response (DTH), a type of cellular immunity that induces the production of two cytokines (proteins that modulate cell function), IFN-γ and TNF-α, that cause macrophages (hosts) infected by the parasite to produce nitric oxide to destroy them.
Individuals classified in the asymptomatic infection and subclinical resistant infection profiles undergo this immune response.
However, those classified in the symptomatic infection and subclinical oligosymptomatic infection profiles do not express DTH and have strong expression of the humoral response (mediated by antibodies such as immunoglobulin IgG) and cytokines such as interleukin-10 (IL-10), which are able to suppress the function of the cytokine IFN-γ and, as a result, deactivate macrophages, leading to parasite multiplication and disease susceptibility.
In contrast, in the case of the indeterminate initial infection profile, which is characterized by a weak immunoglobulin IgG response and negative DTH expression, the immune response of the cases that evolved to asymptomatic infection comprised low production of IL-10, at levels similar to those of cases with subclinical resistant infection profiles.
“The indeterminate initial infection profile performs a pivotal role in the dynamics of infection evolution,” Corbett said. “Based on this profile, the clinical and immunological conditions can evolve towards either the subclinical resistant infection, asymptomatic infection or subclinical oligosymptomatic infection profile, depending on the immunogenetic nature of the individual.”
Of the 23 individuals classified as belonging to the indeterminate initial infection profile, only one evolved to have a symptomatic infection.
The researchers noted that nine cases evolved to subclinical resistant infections, eight remained as indeterminate initial infections and five cases became subclinical oligosymptomatic infections.
“We are proposing additional studies to identify other new immunological markers that could accurately indicate the direction of an indeterminate initial infection,” said Marcia Dalastra Laurenti, a professor at FMUSP and one of the principal researchers on the project. “We will try to identify factors that could predict susceptibility or resistance to the disease.”
The genetic profile of the infected patient may be one of the determining factors in the evolution of the indeterminate initial infection profile to the asymptomatic or symptomatic profile.
Other factors may also contribute to development of resistance to AVL, including exposure to the bite of the female insect vector of the disease—the species Lutzomyia longipalpis—without being infected by L. (L.) i. chagasi.
“Studies indicate that, when exposed to the bite of the non-infected phlebotomine, residents in disease-endemic areas may develop low-level but continuous immunity, which could grant them a certain resistance over time,” said Cláudia Maria de Castro Gomes, an FMUSP researcher and another principal investigator on the project.
New research fronts
On another front, the researchers seek to better understand the immunological factors related to the severity of AVL, in an effort to reduce disease mortality. This study is also included under the thematic project and involves a collaboration with Mônica Gama, professor at the Federal University of Maranhão (UFMA).
The study investigated the relationship between the clinical manifestations—signs of severity defined in a protocol drafted by the Ministry of Health—and the peripheral blood cytokine profile of children who received care through the referral service in Maranhão.
The researchers demonstrated that the severity of the disease is associated with low levels of the cytokine IFN-γ and elevated levels of IL-10.
“The study results showed that IL-10 levels are directly related to the severity of cutaneous visceral leishmaniasis because this cytokine appeared most frequently in children who displayed symptoms of the severe form of the disease,” Gomes said.
The researchers also conducted experimental studies in vitro and in vivo on Neotropical primate species to assess the susceptibility of the animals to L. (L.) i. chagasi infection.
The Sapejus apella monkey presented a specific IgG antibody response beginning three months after infection and positive delayed hypersensitivity test results.
“We observed that primates are good models for further study of resistance to the infection,” Laurenti said.
According to the researchers, Brazil represents one of the largest foci of leishmaniasis in Latin America. More than 90% of all AVL cases, totaling approximately 3,000 cases per year, are reported from this area.
Although the most important features of AVL are understood, the disease is not being effectively controlled due to its clinical and epidemiological complexity.
“Until the 1980s, we observed that visceral leishmaniasis was restricted to the driest areas of Brazil such as the northeast. Today, as a result of factors such as increased urbanization, we are seeing that, despite efforts to control the disease, it is expanding into other areas of Brazil,” Corbett said.
The article, A prospective study on the dynamics of the clinical and immunological evolution of human Leishmania (L.) infantum chagasi infection in the Brazilian Amazon region (doi: 10.1016/j.trstmh.2010.05.002), by Silveira and colleagues may be read in the journal Transactions of the Royal Society of Tropical Medicine and Hygiene at: www.sciencedirect.com/science/article/pii/S0035920310001112.
The article, A cross-sectional study on the clinical and immunological spectrum of human Leishmania (L.) infantum chagasi infection in the Brazilian Amazon region (doi: 10.1016/j.trstmh.2009.06.010), by Crescente and colleagues may be read in the journal Transactions of the Royal Society of Tropical Medicine and Hygiene at: http://trstmh.oxfordjournals.org/content/103/12/1250.abstract?sid=362afa22-bbbd-4c98-9089-f714b064c209.
The article, A longitudinal study on the transmission dynamics of human Leishmania (Leishmania) infantum chagasi infection in Amazonian Brazil, with special reference to its prevalence and incidence (doi: 10.1007/s00436-008-1230-y), by Silveira and colleagues may be read in the journal Parasitology Research at: http://link.springer.com/article/10.1007%2Fs00436-008-1230-y#.
The article, Severe visceral leishmaniasis in children: the relationship between cytokine patterns and clinical features (doi: 10.1590/0037-8682-0203), by Gama and colleagues may be read in the Journal of the Brazilian Society for Tropical Medicine at: www.scielo.br/scielo.php?pid=S0037-86822013000600741&script=sci_arttext.
The article, Susceptibility of Cebus apella monkey (Primates: Cebidae) to experimental Leishmania (L.) infantum chagasi-infection (doi: 10.1590/S0036-46652011000100008), by Carneiro and colleagues may be read in the Journal of the Institute of Tropical Medicine of São Paulo at: www.scielo.br/scielo.php?script=sci_arttext&pid=S0036-46652011000100008.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





