
The combined use of thalidomide and dexamethasone was more efficient in retarding the progression of the disease in transplant patients, indicates studies
The combined use of thalidomide and dexamethasone was more efficient in retarding the progression of the disease in transplant patients, indicates studies
The combined use of thalidomide and dexamethasone was more efficient in retarding the progression of the disease in transplant patients, indicates studies
The combined use of thalidomide and dexamethasone was more efficient in retarding the progression of the disease in transplant patients, indicates studies
By Karina Toledo
Agência FAPESP – A multicenter study conducted by a Brazilian researcher showed that the combined use of thalidomide and dexamethasone in patients with multiple myeloma after undergoing autologous bone marrow transplants was more efficient in retarding the progression of the disease than the single use of dexamethasone.
The study was composed of 213 patient volunteers from four institutions: Universidade Federal do Rio de Janeiro (UFRJ), Faculdade de Ciências Médicas da Santa Casa de São Paulo, Universidade Estadual de Campinas (Unicamp) and Universidade de São Paulo (USP) in Ribeirão Preto.
After 27 months, the study found that 30% of patients who received dexamethasone were still disease free. In the group that received the combination of thalidomide and dexamethasone, that number was more than doubled to 64%. The results were published in the American Journal of Hematology.
Multiple myeloma is a type of cancer that develops within bone marrow due to the uncontrolled growth of plasmocytes, cells responsible for producing antibodies. The disease harms the production of erythrocytes, causing anemia, and favors the release of substances that weaken bones.
“Although there is no cure, the newest treatments are managing to greatly retard the cancer’s progression. Myeloma today could become a chronic disease,” says Angelo Maiolino, professor at UFRJ and lead author of the study.
The treatment that is currently considered the gold standard, explains the researcher, involves chemotherapy and antineoplastics, such as bortezomib, in addition to autologous bone marrow transplants, which are performed with cells from the patient, and a maintenance therapy with medication that modulates the immunological system, such as corticoids and thalidomide.
“Only 30% of patients, however, are suited for the transplants, which is only recommended for people aged 65 and under. The other 70% must be treated only with medication, “ explains Maiolino.
According to the researcher, when the study was idealized almost 10 years ago, administering maintenance therapy after a transplant was still not common. “Thalidomide was used only in cases of a relapse of the disease. Our objective was to investigate whether it would also offer benefits if used to retard the reappearance of cancer,” he explained.
During the period in which this study was conducted, six other studies were published in several countries evaluating the efficacy of thalidomide as maintenance therapy. “Some compared it with another type of corticoid, such as prednisone, others with interferon, and others with a placebo. All concluded that thalidomide increased the progression-free survival of patients,” explains Maiolino.
In addition to acting directly on plasmocytes, impeding connection to the bone marrow, the drug inhibits the formation of blood vessels that supply malignant cells, which end up dying.
“Thanks to the new combinations of medicine, it was possible to increase progression-free survival from three to eight years in the last decade. It seems like very little, but it is a considerable leap when it involves cancer,” says Maiolino.
In the researcher’s opinion, the future trend is for thalidomide to be substituted in maintenance therapy for lenalidomide, which is in the same class of drugs but is a second-generation medication offering fewer side effects.
“Sooner or later, the prolonged use of thalidomide causes peripheral neuropathy, an inflammation of the nerves that limits use of the medication. As this does not occur with lenalidomide, it can be used for longer. However, unfortunately, this medicine is not yet approved in Brazil,” said Maiolino.
Thematic Project
In addition to the four university centers, the study coordinated by Maiolino also boasted the participation of the National Cancer Institute’s (Inca) Bone Marrow Transplant Center and funding from FAPESP and CNPq.
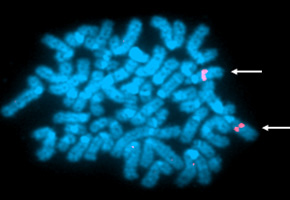
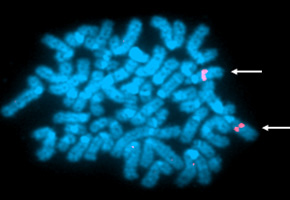
“All of the cytogenetic part, which investigated chromosomal mutations that allow for the determination of patient prognosis, was conducted with FAPESP funding. The objective was to discover if the results are influenced by unfavorable genetic alterations, but we saw that this did not occur,” explains Vânia Tietsche de Moraes Hungria of the Santa Casa de São Paulo Medical Sciences School.
The study was conducted under the auspices of a Thematic Project coordinated by Carmino Antonio de Souza at Unicamp.
According to Maiolino, the study has symbolic importance because clinical studies conducted completely in Brazil without any pharmaceutical industry support are still rare. “There are various multicenter studies on myeloma underway in the country, but they came from abroad and are sponsored,” he said.
The article “Thalidomide plus dexamethasone as a maintenance therapy after autologous hematopoietic stem cell transplantation improves progression-free survival in multiple myeloma” can be read at http://onlinelibrary.wiley.com/doi/10.1002/ajh.23274/abstract;jsessionid=CA35A005BCBC9A88755F7A3C09BFB904.d03t02.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





