
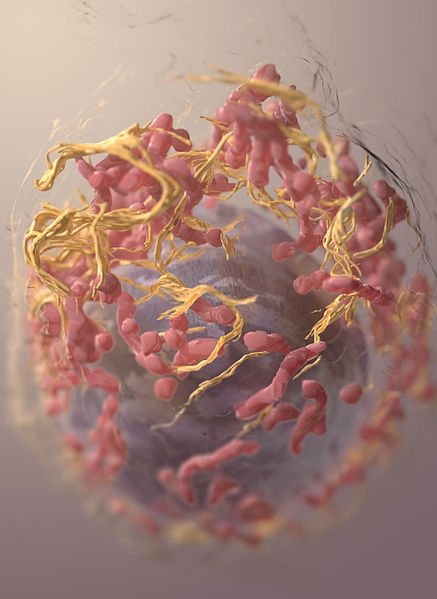
In a presentation to the 8th Workshop on Melanoma Models, British scientist Colin Goding spoke about how a lack of nutrients can make tumor cells stop proliferating and acquire an invasive phenotype (image: Sriram Subramaniam, National Cancer Institute (NCI), 2012 / Wikimedia Commons)
In a presentation to the 8th Workshop on Melanoma Models, British scientist Colin Goding spoke about how a lack of nutrients can make tumor cells stop proliferating and acquire an invasive phenotype.
In a presentation to the 8th Workshop on Melanoma Models, British scientist Colin Goding spoke about how a lack of nutrients can make tumor cells stop proliferating and acquire an invasive phenotype.
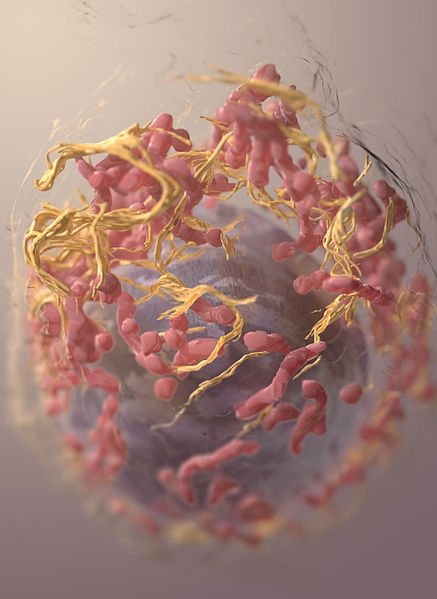
In a presentation to the 8th Workshop on Melanoma Models, British scientist Colin Goding spoke about how a lack of nutrients can make tumor cells stop proliferating and acquire an invasive phenotype (image: Sriram Subramaniam, National Cancer Institute (NCI), 2012 / Wikimedia Commons)
By Karina Toledo | Agência FAPESP – British researcher Colin Goding is convinced that just as the first single-cell living organism ever to move over 3 billion years ago was motivated by the search for food, the same factor is also the reason why some tumor cells separate from a primary tumor to colonize other parts of the body.
In experiments with cultured human melanoma cells conducted at his laboratory at the Ludwig Institute for Cancer Research based at the University of Oxford in the United Kingdom, Goding has shown that a lack of nutrients deactivates the cell proliferation machinery and induces tumor cells to acquire an invasive phenotype.
“We believe the same logic may operate for most types of cancer, and we may be able to find ways to manipulate this cellular survival mechanism to obtain therapeutic benefits,” Golding told Agência FAPESP.
During a visit to São Paulo, where he delivered the opening presentation to the 8th Workshop on Melanoma Models on August 10, Goding explained that his group has used melanoma as a model to understand the progression of cancer in general.
“Melanoma is a very good model to study cancer because we can see all stages of the disease,” he said. “We can see when pigment cells start to invade other tissue and form metastases. In other kinds of cancer, such as lung cancer or pancreatic cancer, when the symptoms appear and the patient goes to a doctor, the tumors have already spread.”
Another factor that has made melanoma an interesting model for studying cancer, according to Goding, is the identification over a decade ago of a gene called BRAF, which is activated in approximately 50% of melanomas and stimulates uncontrolled cell proliferation.
“Within a few years, there were drugs targeting specifically the activated form of BRAF with dramatic results. Patients with multiple metastases respond incredibly well to BRAF inhibitors,” Goding said. “However, after a few months, the cells become drug-resistant. The question we asked was why this resistance develops and what we can do about it.”
Change of phenotypic state
According to Goding, recent research has shown that treatment resistance in melanoma is linked to the existence of cell populations with different phenotypes in the same tumor. These subpopulations have the same genetic background, but behave differently.
“Some may be more differentiated, reflecting the tissue of origin, so these are more pigmented cells. Some will be proliferating and making the tumor grow. Some become invasive, and so you start to see metastases. Some become dormant, so that even after a successful therapy, the same disease may reappear many years later,” Goding explained.
One of the British group’s aims therefore has been to understand the factors that lead to the appearance of these different phenotypes. According to Goding, aspects of the tumor microenvironment, such as the availability of nutrients, oxygen levels and interactions with signals emitted by the immune system, influence the switch from one phenotypic state to another.
The hypothesis raised by Goding is that nutrient limitation within a tumor activates a survival mechanism in its cells that makes them seek nutrients elsewhere.
“We also believe certain signals from immune cells, such as the cytokines TNF-α [tumor necrosis factor alpha] and TGF-β [transforming growth factor beta], may lead to a pseudo-starvation state. There may be plenty of nutrients around, but these immune signals associated with inflammation can engage the same starvation mechanism within the cell and that then induces the cell to start moving,” he said.
Experiments performed by Goding with yeast, fungi and melanoma cells have confirmed the conservation of this cell survival mechanism throughout evolution. Starvation makes cells reduce their demand for nutrients to match the decrease in supply. This means deactivating the biological processes required to synthesize proteins for the formation of new cells.
However, when tumor cells are able to migrate to a new environment where there are plenty of nutrients and no immune cells inducing pseudo-starvation, they start proliferating again and metastasis results.
“If we can trick cells into thinking the hypoxia, starvation and other stress signals have gone away, they will reactivate the machinery to build new cells and then they will die because their demand for nutrients will greatly exceed the supply,” Goding said.
The manipulation of phenotypic states in tumor cells, he added, could theoretically prevent both the formation of metastases and future relapses of the disease.
“The process of metastasis formation is very inefficient,” he said. “There must be hundreds of thousands of tumor cells in circulation, but only a few succeed in establishing a new colony. Some of these cells die. Some become dormant to survive the stress associated with escape from the primary tumor. If we can find a way to eliminate this dormancy, we can reduce still further the percentage of cells that manage to escape from the primary tumor, survive, and form metastases. This is something we’re pursuing in my lab, in collaboration with groups worldwide, including Silvya Stuchi and her group here in Brazil.”
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





