
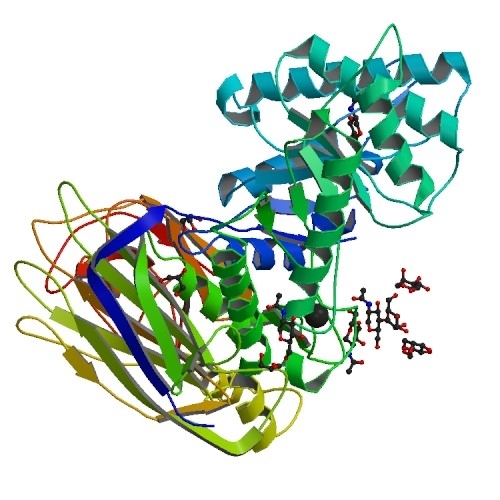
Mucopolysaccharidosis is caused by mutations in a single gene that encodes the enzyme alpha-L-iduronidase (IDUA) (image: Protein Data Bank)
Treatment with genetically modified mesenchymal stem cells improved cognitive performance in experiments with mice.
Treatment with genetically modified mesenchymal stem cells improved cognitive performance in experiments with mice.
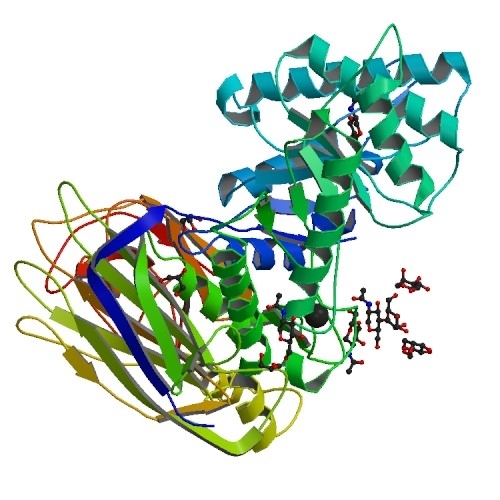
Mucopolysaccharidosis is caused by mutations in a single gene that encodes the enzyme alpha-L-iduronidase (IDUA) (image: Protein Data Bank)
By Karina Toledo
Agência FAPESP – Researchers at the Biophysics Department of the Federal University of São Paulo (UNIFESP) in Brazil are developing a gene therapy for mucopolysaccharidosis type I (MPSI), a genetic disease that causes cognitive impairment and injuries to several organs.
The research is supported by FAPESP and coordinated by Professor Sang Won Han.
“The treatment currently available is enzyme replacement therapy,” he said. “This is lifelong therapy, and it’s costly. It can’t reverse cognitive damage, but only slows down its progression. Bone marrow transplants are an option; however, it’s difficult to find compatible donors, and the procedure must be performed in the first few years after birth. We’re trying to find a cure via gene therapy. We’ve already observed an improvement in experiments with mice.”
The disease, he explained, is caused by a mutation of the gene encoding alpha-L-iduronidase (IDUA), an enzyme responsible (along with other proteins) for the degradation of glycosaminoglycans (GAGs), which are polysaccharides with important functions throughout the body.
“GAGs are components of the extracellular matrix and perform key roles outside and inside cells, including signal transduction,” Han explained. “Like any other macromolecule, however, GAGs eventually need to be recycled. IDUA deficiency results in a failure of this process, so GAGs build up in cells, affecting their functions and potentially leading to cell death.”
Without treatment, the patient’s organs begin to swell, and their functioning is impaired. The spleen and liver are usually the worst affected, but the heart, brain, joints and bones also suffer.
The main treatment available at present is IDUA enzyme replacement, which must be intravenously administered every week at a hospital. The annual cost to Brazil’s national health service (Sistema Único de Saúde, SUS) is more than US$100,000 per patient.
Scientists are not sure whether the recombinant enzyme crosses the blood-brain barrier, a mass of endothelial cells that protect the central nervous system, but the fact is that enzyme replacement therapy in its present form is unable to reverse a patient’s brain damage. Moreover, some patients suffer severe side effects due to their immune system’s response to infusion of the enzyme.
The researchers, led by Han, as well as other groups in different parts of the world, are seeking a method of inserting a functional copy of the IDUA gene into the patient’s genome so that the patient’s own cells can produce the molecule in a sustained manner.
Stem cells
Two strategies were tested in experiments with mice at UNIFESP. The IDUA gene was inactivated, or “knocked out,” and the mice developed a condition similar to MPSI.
In one experiment, the researchers isolated and modified mouse bone marrow mesenchymal stem cells (MSCs) using a virus as the vector. This material was injected into the brains of the knockout mice.
“We removed the viral genome and put a copy of the human IDUA gene in its place,” Han said. “When a cell is infected by this modified virus, the gene of interest integrates with its genome, and the cell begins to produce the enzyme.”
MSCs are multipotent stromal cells that migrate to sites of inflammation, such as tissues with a buildup of GAGs. Although MSCs are unlike embryonic stem cells in that they cannot differentiate into all cell types, they are considered interesting from a therapeutic standpoint because of their properties, which range from anti-inflammatory and anti-apoptotic (prevention of cell death) to immunomodulatory. In addition, like all stem cells, they are capable of self-renewal.
The modified cells were injected into the left brain ventricle, and the animals’ cognitive performance was evaluated by means of behavioral tests for one to two months.
“We observed a significant improvement in cognitive functions in tests designed to evaluate exploratory capacity,” Han said. “We believe any treatment for the brain must be administered separately.”
Brain tissue analysis showed a significant reduction in GAG deposition in treated mice compared with the control group of untreated mice. However, IDUA production was not significant in the brain tissue samples analyzed after the two-month observation period.
“A small number of modified MSCs were left in the tissue after this period, but it was possible to observe that they had in fact migrated to the other side of the brain, promoting an overall improvement,” Han said.
The results, obtained during Flávia Helena da Silva’s PhD research under the supervision of Han and Nance Nardi, a professor at the Lutheran University of Brazil, were described in an article published by the journal Genetic Vaccines and Therapy.
Hydrodynamic injection
A different approach tested during Roberta Sessa Stilhano Yamaguchi’s research for her master’s degree, supported by a scholarship from FAPESP, involved the insertion of human IDUA genes into plasmids, or circular DNA molecules taken from bacteria.
“We opted for a plasmid vector with a view to clinical use because plasmids are safer to use as vectors than viruses are,” Han said. “To engineer the plasmid vector, we took a recombinase-encoding gene from the Streptomyces bacteriophage phiC31, which helps integrate the gene of interest into the target cell’s genome to ensure lasting production of the enzyme.”
A large amount of plasmid solution, corresponding to 10% of the animal’s body mass, was injected into the tail vein. This method, known as hydrodynamic injection, forces vector DNA into blood cells by hydrostatic pressure, and from there it spreads to other parts of the body.
“In humans, the method would have to be somewhat different,” Han said.
Following vector injection, production of IDUA jumped from practically nil to 1,000 units per milliliter of blood. However, about a month later, it had returned to the initial level. The results were described in an article published by The Journal of Gene Medicine.
“The problem is that the murine organism identifies the plasmid as a foreign body and neutralizes the treatment by generating antibodies against human IDUA and silencing gene expression by epigenetic mechanisms such as DNA methylation,” Han said. “We’re now attempting to circumvent this problem in the lab by means of genetic engineering.”
During Priscila Keiko Matsumoto Martin’s research for her master’s degree, supported by FAPESP, the group tested a method for circumventing this immune response using MSCs modified with a plasmid vector containing the genes for IDUA and SB transposase, which also integrates the gene of interest into the host cell’s genome. “MSCs are known to have immunosuppressive properties, so we expected to circumvent the immune response, but enzyme production was negligible. We discovered that MSCs are not an ideal immunosuppressant in our case, which relates to antibody production,” Han said.
The results were described in an article published by PLOS ONE and presented in September at the 30th Annual Meeting of the Brazilian Federation of Experimental Biology Societies (FeSBE), held at the University of São Paulo’s School of Medicine (FM-USP).
“Our next step is to improve the vector by using a DNA fragment that more closely resembles mammalian DNA to mitigate the problem of epigenetic gene silencing,” Han said. “In humans, the immune response is highly likely to be weaker, as the enzyme produced will also be human. Many MPSI patients do actually produce IDUA: it’s defective, i.e., non-functional, but the organism is accustomed to it.”
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





