

First-ever study to show correlation between inhibition of protein HSP70 and dysfunction of cells in inner lining of blood vessels, one of the factors involved in chronic thromboembolic pulmonary hypertension (image: Thaís Araujo & Luiza Coimbra/USP)
First-ever study to show correlation between inhibition of protein HSP70 and dysfunction of cells in inner lining of blood vessels, one of the factors involved in chronic thromboembolic pulmonary hypertension.
First-ever study to show correlation between inhibition of protein HSP70 and dysfunction of cells in inner lining of blood vessels, one of the factors involved in chronic thromboembolic pulmonary hypertension.
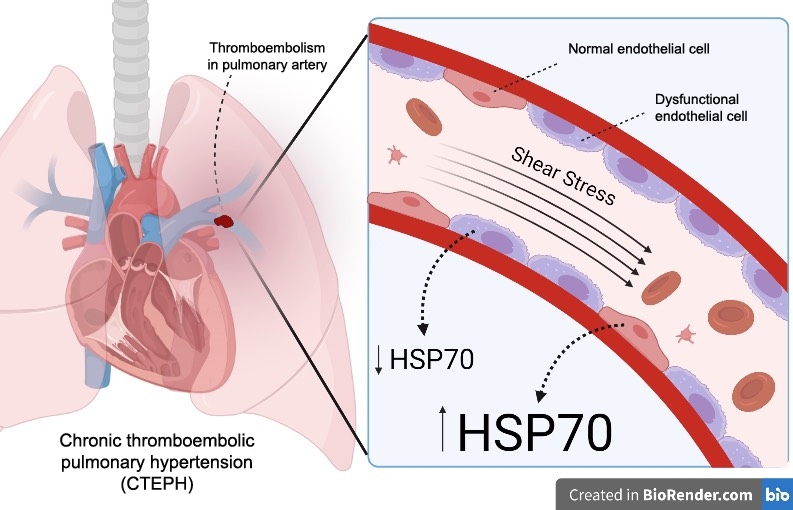
First-ever study to show correlation between inhibition of protein HSP70 and dysfunction of cells in inner lining of blood vessels, one of the factors involved in chronic thromboembolic pulmonary hypertension (image: Thaís Araujo & Luiza Coimbra/USP)
By Karina Ninni | Agência FAPESP – Chronic thromboembolic pulmonary hypertension (CTEPH) is a relatively rare vascular disease caused by blood clots (thrombi) in the lungs that are not cleared by anticoagulant medicine. The obstruction due to the clotting eventually overloads the right ventricle of the heart. Treatment can involve surgery (pulmonary thromboendarterectomy, PTE) to remove clotted blood from arteries in the lungs, but not all patients are eligible. Some 35% continue to suffer from the disease after the operation.
“In 35% of patients, we remove the clotted blood but pressure in the arteries of the lungs remains high, suggesting there’s something else wrong apart from the clotting,” said William Salibe-Filho, a pulmonologist at the Heart Institute (INCOR) of Hospital das Clínicas (HC), the hospital complex run by the University of São Paulo’s Medical School (FM-USP) in Brazil.
With FAPESP’s support, Salibe-Filho, Thaís Larissa Araújo, a biophysicist at the Institute of Chemistry (IQ-USP) and other collaborators investigated the endothelial cells of the pulmonary arteries in search of answers.
“The inner walls of the arteries in the lungs are lined with a single layer of endothelial cells. What’s fairly well-established about the disease is that the functioning of these endothelial cells is impaired and the heart has to work a lot harder as a result,” Salibe-Filho explained. “The right side of the heart has to pump more blood to overcome the resistance and bad circulation in the lungs. Patients eventually suffer from heart failure, but it’s the right side of the heart that’s affected.”
In an article published in the journal PLOS ONE, the scientists reported that dysfunctional endothelial cells expressed too little HSP70, a protein that helps others acquire the right structural configuration for the performance of their functions. Such proteins are known as molecular chaperones. The authors argue that HSP70 regulates endothelial dysfunction and shows significant potential to be a biomarker of the disease.
“We previously studied the behavior of chaperones in response to shear stress, a dynamic force that happens naturally as blood flows through vessels and can be more or less intense in the arteries,” Araújo said. “In earlier research, we observed that HSP70 levels were low where the shear stress was low. That was the first time anyone had demonstrated the correlation, showing that there was less HSP70 in areas with less flow shear stress and that this was associated with atherosclerosis and endothelial dysfunction. In other words, we had already produced evidence of the link with chaperone reduction in the cardiovascular system.”
In the specific case of blood flow in pulmonary arteries, low shear stress is the ideal. “When this disease is present and clotting occurs, blood flow is low where it’s obstructed but elsewhere it increases and becomes very intense. Endothelial cells respond badly. But we didn’t know exactly which proteins were involved in this process. For the first time, we showed molecularly that certain proteins are key to this endothelial dysfunction,” Araújo said.
Endothelium
According to Salibe-Filho, the group of patients with CTEPH is not very large and is considered part of a broader community with diseases generically classified as due to pulmonary hypertension (PH). There are four other groups in this community: patients with PH directly due to hardening of the arteries in the lungs, those with heart failure (the most common type of pulmonary hypertension), those with pulmonary lesions, and those with PH due to multiple mechanisms involving hematological, systemic and/or metabolic disorders. “Endothelial dysfunction is present to a greater or less extent in almost all these groups,” he said.
Patients who have had an acute pulmonary embolism usually develop CTEPH. A small proportion (4%-5%) eventually develop chronic pulmonary embolism. “We wondered what was different about the patients who progressed to CTEPH, and decided to study endothelial dysfunction in these specific patients,” Salibe-Filho said.
Araújo explained that endothelial cells are the first to have contact with the blood as it flows through a vessel. Fluctuations in hemodynamic force, where the flow is less intense or turbulent, will be “sensed” or “seen” at first hand by the endothelial cells. “For this reason, they’re important to the vascular modeling response. We wanted to find out what happens to chaperone expression in patients with endothelial dysfunction,” he said.
Salibe-Filho summed up the group’s discoveries. “We knew dysfunctional endothelial cells filled these patient’s blood vessels differently and were unable to maintain the function they performed previously. We discovered that this is partly regulated by chaperones.”
Methods
According to the researchers, the advantage of studying CTEPH patients was that tissue samples from them were available because they had been operated on. “If we studied other groups, we wouldn’t have the tissue sample, because surgery isn’t applicable to the other groups,” Salibe-Filho said. “We developed a technique to extract cells from the endothelium of this tissue. It isn’t a simple process. We isolated, characterized and cultured them, and then we tried to simulate shear stress in vivo.”
They analyzed endothelial cells from the thrombi of seven CTEPH patients submitted to surgery at INCOR. These cells, as well as commercially acquired control cells, were exposed to high and low shear stress (15 dynes/cm2 and 5 dynes/cm2 respectively. A dyne is a unit of force defined as equal to the force that would give a free mass of one gram an acceleration of one centimeter per second per second).
“When we applied high shear stress to cells from CTEPH patients, we were unable to increase the expression of HSP70. In control cells, we succeeded in doing so,” Araújo said.
Less expression of HSP70 under high shear stress results, among other things, in less migration of endothelial cells and less vascular tube formation.
“We also used an HSP70 inhibitor and found that tube formation [angiogenesis] and cell migration were even more reduced. This enabled us to observe even more clearly the correlation between low chaperone presence and low capacity for migration and angiogenesis. In other words, we showed a direct correlation between the function of HSP70 and endothelial dysfunction,” Araújo said.
Future
According to the scientists, in future these discoveries can contribute to the development of treatments targeted to each case of PH. “Specific vasodilator medications are used at present,” Salibe-Filho said. “CTEPH is the only case in which surgery is possible, and even so only after three months of treatment with anticoagulants. More precise or rapid diagnosis may be possible with a biomarker, or it may be possible to know via a biomarker whether a patient will progress to a more severe condition and require intervention sooner. These are hypotheses that require further study, but we believe our discoveries open up such possibilities.”
For Araújo, the possible discovery of a biomarker is key to better treatment of the disease insofar as it facilitates prognosis. “A biomarker could be the precursor of a decision to operate by helping the medical team determine whether the intervention is worthwhile,” she said. “If this correlation between low chaperone expression and endothelial dysfunction can be detected early enough, it may be inappropriate to prescribe surgery because removal of the thrombus might not resolve the matter in cases where clotting isn’t the only problem.”
The study was funded by FAPESP via six projects: 18/13739-8, 19/20435-8, 15/06210-2, 20/11249-3, 19/25503-1 and 13/07937-8.
The article “Shear stress-exposed pulmonary artery endothelial cells fail to upregulate HSP70 in chronic thromboembolic pulmonary hypertension” is at: journals.plos.org/plosone/article?id=10.1371/journal.pone.0242960.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





