
The average time between the emergence of the lesions and a definitive diagnosis is more than four years.
The average time between the emergence of the lesions and a definitive diagnosis is more than four years.
The average time between the emergence of the lesions and a definitive diagnosis is more than four years.
The average time between the emergence of the lesions and a definitive diagnosis is more than four years.
By Noêmia Lopes
Agência FAPESP – Melanoma is a neoplasia (cancer) with origins in pigment production cells. Although it can also appear in mucous glands, the absolute majority of cases occur in the skin and are termed primary cutaneous melanoma. This type of neoplasia manifests in different ways, and the symptoms have a direct relationship to the prognosis and treatment of the disease.
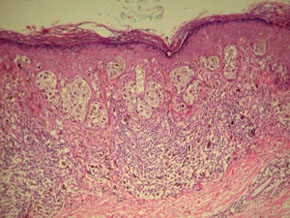
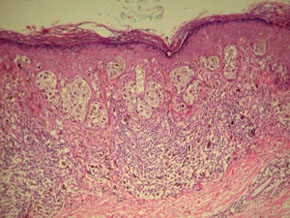
Classifying a melanocytic lesion (pigmented) as benign, malignant or a suspected malignancy requires a combination of clinical observations conducted during medical consultations and histological analyses and investigation of the lesion with the help of microscopes.
When a lesion is malignant, the main indicator of the prognosis is the Breslow Index, which relates the vertical depth (tissue invasions) of the melanoma in millimeters to the severity of the case and the probability of metastasis. However, countering the scales, there are cases of patients with deep tumors and better survival rates as well as small tumors that grow aggressively with a tendency to metastasize.
In this scenario, knowledge of a second widely used resource for the analysis of lesions should be broadened: immunohistochemical markers of tumor progression, which are the focus of a study developed at Universidade Estadual Paulista’s Botucatu School of Medicine (FMB/UNESP) with the support of FAPESP and the approval of the FMB Ethics Committee. “Immunohistochemical markers are specific antibodies – anti-Bcl-2, anti-p53, anti-Ki-67 and HMB-45, in the case of this study – which react with the tissue analyzed if the antigens against which they were produced are present, establishing an antigen-antibody connection,” said Sílvio Alencar Marques, full professor at the Dermatology and Radiotherapy Department at FMB, who is responsible for the study.
Marques, two other researchers – Mariangela Marques, a professor in the Pathology Department, and Ana Claudia Cavalcante Espósito, a resident doctor in the Dermatology and Radiotherapy Department at FMB and a FAPESP fellow during the study – and engineer Felipe Kesrouani Lemos, responsible for the statistical data analysis, started from the premise that assembling a broad panel of immunohistochemical markers could create in an important aid in diagnosing lesions.
The study began with clinical and demographic examinations of 195 patient files at FMB – all with melanomas surgically removed by the Dermatology Clinic and analyzed by the Pathology Department from 2000 to 2010. This stage allowed them to reach their first and alarming conclusion regarding the group of people studied: the average time between the appearance of the lesions and diagnosis was 4.04 years.
“This interval is frightening and has a very negative impact on the prognosis of the cases. Moreover, it shows the lack of health education on the part of individuals who are likely to develop melanoma – those with very light skin and with many nevi (also called moles) - and the probable lack of medical knowledge on the suspected signs of malignant lesions,” said Marques.
The second part of the study involved an analysis of the melanomas. To do so, scientists separated the biopsies into four main subtypes: 1) extensive superficial melanoma, in theory the best prognosis because it tends to grow slowly and invade tissue later; 2) lentigo maligna melanoma, which occurs in light-skinned senior citizens in areas exposed to the sun and in theory also carries a good prognosis because of its horizontal growth over long periods before invading tissue; 3) acral lentiginous melanoma, found on the palms of the hands, on the soles of the feet and under nails among Black and interracial individuals and people of Asian descent; 4) nodular melanoma, which carries the worst prognosis because it rapidly invades the deepest tissues of the skin and causes precocious metastasis.
After splitting cases into these categories, the researchers chose a number to represent each subtype and conducted immunostaining. In effect, anti-Bcl-2, anti-p53, anti-Ki-67 and HMB-45 were applied to samples so that the team could evaluate their respective reactions. “We utilized a technique called avidin-biotin-peroxidase in which the coloration of a cell that has been marked positive turns dark brown, in contrast to unmarked cells, which remain light blue,” commented Marques.
The Bcl-2 paradox
After the tissues were cut into thin sections and stained, the reactions were compared and studied. During this stage, some of the study’s initial hypotheses regarding apoptosis were ruled out. Apoptosis, or programmed cell death, is set in motion to rapidly and efficiently eliminate unnecessary or damaged cells.
Cells that have DNA alterations, either because of metabolic or oncogenic stress (involving tumors), increase the production of a protein called p53, which leads to the induction of genes that suppress tumors through apoptosis. This explains the rationale that p53 is pro-apoptotic.
Cancer is the result of uncontrolled cellular proliferation, and cancerous cells develop systems to disarm apoptosis and ease the progression and persistence of the disease. This occurs through the inhibition of p53 function or an increase of Bcl-2, another anti-apoptotic protein.
“One would expect, therefore, that in melanomas, principally those with a high rate of cellular proliferation, immunostaining of Bcl-2 would be expressive. However, that is not what many articles in the literature show, and it was also not what we observed,” commented Marques.
“Moreover, among the subtypes of melanoma, Bcl-2 was more striking in extensive superficial melanomas than in nodular melanomas. In this last and more aggressive subtype, one would expect a greater presence of the anti-apoptotic protein,” she explained.
The researchers still do not have definitive explanations for this paradox. One hypothesis is that other anti-apoptotic proteins in the Bcl-2 family may compensate for the “immortalization” role of Bcl-2 itself, and therefore, Bcl-2 is not expressed as expected.
“The definitive diagnosis still falls on the expertise of clinicians and pathologists. Auxiliary methods need more investigation and technological implements. Additionally, there is a need to search for other more sensitive and specific markers,” explained Marques.
Developments
Faced with the 195 diagnoses performed in the FMB’s Dermatology Clinic over a decade, the researchers verified that melanoma cannot be considered a rare infirmity, and on the contrary, has been growing quantitatively. “This observation has prompted a parallel study that proved, given the parameters of comparison, that the incidence of skin cancer is on the rise. Specifically, there was a 171% increase from 1999 to 2011,” explained Marques.
Another rate that is on the rise is the frequency of acral lentiginous melanoma, which has grown by 13%. Occurring in brown and Asian-toned skin, this type poses additional challenges in clinical diagnosis because it is less known by general practitioners and therefore has higher chances of late diagnoses. Health education for patients and refresher courses and training for doctors are among the practical steps proposed by the study.
Considering the major gap between the perception of the lesion and the definitive diagnosis, the researchers intend to produce and distribute informative folders and promote courses and events that cover the melanomas and their main warning signs. According to Marques, “the intention is that the suspicion and diagnosis occur at the earliest moment possible.”
One likely deficiency between doctors could be related to the knowledge and interpretation of the method known as ABCDE, in which A corresponds to the asymmetry (healthy nevi have horizontally and vertically symmetrical halves), B to the borders (normal nevi have regular limits), C to the color (in general, nevi have a homogenous color, whereas melanomas have more than one coloration on the surface), D to diameter (lesions of over six millimeters should be considered suspicious) and E to the evolution (modifications in pre-existing moles).
“All doctors should know these rules. They are not absolute, but they work exceptionally well for the first screening,” said Marques. Also with the objective of accelerating the diagnosis time, the study proposes that the FMB improves patient files (now electronic) and the protocols used for melanoma cases – if faithfully followed by the institution’s dermatological oncology team, it will contribute to the research of the team that is now focused on evaluating immunostaining in metastasis.
The results of the study have been presented at two conferences: Espósito gave an overview to FMB’s Academic Medical Congress in 2012, and Marques spoke at the 31st Annual Meeting of Latin-American Dermatologists (31st Radla) in April 2013 in Uruguay. In addition to the researchers directly involved in the study, the team credits the indirect participation of lecturers, doctors and residents who diagnosed and removed lesions at the FMB over the last decade.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





