

Studies in mice suggest that two drugs capable of inhibiting the enzyme TrxR-1 – already available commercially for other purposes – reduce inflammation and mortality in patients with sepsis (image: confocal microscopy image of leukocyte during in vitro trial)
Studies in mice suggest that two drugs capable of inhibiting the enzyme TrxR-1 – already available commercially for other purposes – reduce inflammation and mortality in patients with sepsis.
Studies in mice suggest that two drugs capable of inhibiting the enzyme TrxR-1 – already available commercially for other purposes – reduce inflammation and mortality in patients with sepsis.
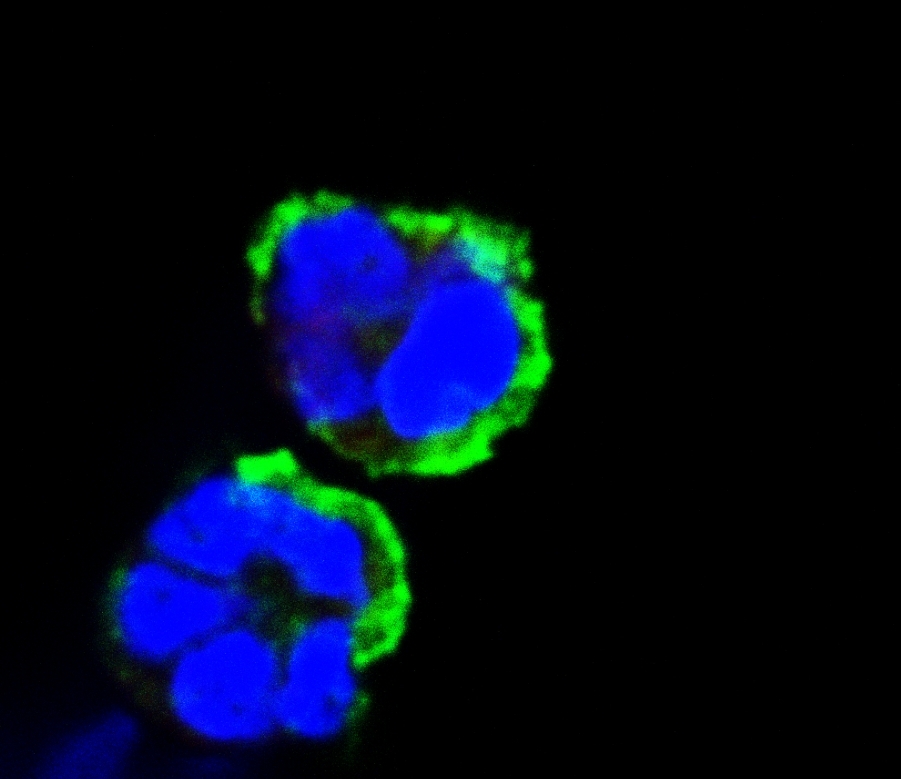
Studies in mice suggest that two drugs capable of inhibiting the enzyme TrxR-1 – already available commercially for other purposes – reduce inflammation and mortality in patients with sepsis (image: confocal microscopy image of leukocyte during in vitro trial)
By Karina Toledo | Agência FAPESP – In an article published in October in the journal Scientific Reports, Brazilian researchers describe a novel strategy to combat inflammation and reduce mortality among patients with sepsis based on inhibition of an enzyme called thioredoxin reductase-1 (TrxR-1).
Two drugs with this activity are commercially available but prescribed for different uses. Auranofin is currently used to treat rheumatoid arthritis, and lanthanum chloride is used to treat kidney failure. Tests in mice showed that these drugs improved survival in sepsis by 50%.
The investigation was conducted during Silvia Cellone Trevelin’s PhD research, with a scholarship from FAPESP and supervision from Fernando de Queiroz Cunha and Lucia Rossetti Lopes, researchers at the Center for Research on Inflammatory Diseases (CRID) and the Center for Research on Redox Processes in Biomedicine (Redoxoma), respectively. Both of these centers are funded by FAPESP under its Research, Innovation and Dissemination Centers (RIDCs) program.
“Our results show that the enzyme thioredoxin reductase may be a new therapeutic target for the treatment of sepsis,” Lopes told Agência FAPESP. “However, the strategy must now be tested in human patients by means of a clinical trial designed to demonstrate its efficacy and explore any deleterious effects.”
According to Cunha, both research groups are engaged in talks with pharmaceutical companies to find ways of testing the strategy in patients with sepsis. “Data from in vitro experiments suggest the strategy could also be worth exploring in the treatment of chronic granulomatous disorder (CGD), a genetic defect that prevents the organism from producing free radicals of oxygen, which are important to combat infections,” he said.
Bacterial infection
Popularly known as “blood poisoning,” sepsis is a potentially life-threatening type of systemic inflammation and a leading cause of death in intensive care units worldwide.
The exacerbated inflammation associated with sepsis is usually triggered by bacterial infection and may remain active even after the pathogen has been eliminated, producing changes in body temperature, arterial blood pressure, heart rate, white blood cell count and breathing. The most severe form of sepsis, known as septic shock, can cause several organs to fail.
According to Cunha, these adverse effects are the result of tissue damage due to overproduction of inflammatory substances, especially the cytokine tumor necrosis factor alpha (TNF-α), by defense cells.
“The body’s defense cells contain a protein complex called nuclear factor kappa B, or NF-κB, which acts as a transcription factor for several inflammatory mediators. It’s normally located in the cytoplasm. When free radicals of oxygen are produced by cells after they come into contact with a pathogen, NF-κB is translocated into the nucleus, where it may bind to DNA and activate cytokine transcription,” said Cunha, who besides heading CRID is a professor at the University of São Paulo’s Ribeirão Preto Medical School (FMRP-USP).
Initially, the researchers thought that eliminating the production of free radicals would be a good strategy to reduce inflammation because, in theory, NF-κB should no longer migrate to the cell nucleus. They tested this hypothesis in mice genetically modified not to express the enzymes that produce free radicals. To their surprise, all the animals died as a result of the inflammation, even when challenged with components of dead bacteria incapable of causing a genuine infection.
“In partnership with the team at Redoxoma, we discovered that inhibiting the production of oxygen radicals was a bad idea for two reasons: first, because they’re important to kill bacteria, and second, because they oxidize TrxR-1, preventing it from translocating to the nucleus and converting NF-κB into the form that induces the production of inflammatory mediators. So, while free radicals can cause damage, they also help balance inflammation during sepsis,” Cunha said.
Based on these findings, the researchers decided to test TrxR-1 inhibition as a therapeutic strategy. In a murine model, systemic inflammation was induced by cecal ligation and puncture (CLP), a procedure that involves puncturing the cecum, part of the large intestine, and allowing feces and intestinal bacteria to spill into the peritoneal cavity.
Half the mice were treated with antibiotics and displayed a survival rate of about 50%. The other half received TrxR-1-inhibiting drugs as well as antibiotics. The survival rate for this group rose to 80%.
Testing in leukocytes
Results of in vitro experiments suggest that the same approach can be used to treat CGD. According to Cunha, patients with this genetic disease do not express the enzymes required for the production of oxygen radicals and are therefore prone to recurring infections and chronic inflammation.
“The organism of a patient with CGD can’t kill pathogens, so it surrounds them with inflammatory cells to form cysts or granulomas. The aim is to keep the pathogen isolated and prevent it from circulating freely. However, recent research has shown that these granulomas often don’t contain bacteria, yet even so, there is inflammation,” he said.
Patients with CGD rarely reach adulthood, either because of recurrent infections or owing to excessive inflammation. “It occurred to us that by inhibiting TrxR-1, we could reduce inflammation and the damage it causes,” he added.
The hypothesis was tested in white blood cells from patients with CGD by stimulating the cells with bacterial components and then incubating them with lanthanum chloride. The TrxR-1-inhibiting drug considerably reduced the production of TNF-α, the key inflammatory mediator underlying the formation of granulomas.
The researchers stressed that this drug has been approved for human use in Brazil since 2013. In Europe and the US, it has been used by patients with kidney failure for about six years, without significant adverse side effects.
“The dose required to inhibit TrxR-1 is less than the dose used to treat kidney failure, so adverse side effects would be even less likely to occur. We therefore believe the conditions exist to commence clinical trials,” Cunha said.
The article “Apocynin and Nox2 regulate NF-κB by modifying thioredoxin-1 redox-state” (doi: 10.1038/srep34581) can be read at nature.com/articles/srep34581.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





