
A study conducted at Unicamp and published in Blood magazine shows that the drug used in the chronic treatment of the disease can also provide relief for acute occlusive vessels, which are currently untreatable.
A study conducted at Unicamp and published in Blood magazine shows that the drug used in the chronic treatment of the disease can also provide relief for acute occlusive vessels, which are currently untreatable.
A study conducted at Unicamp and published in Blood magazine shows that the drug used in the chronic treatment of the disease can also provide relief for acute occlusive vessels, which are currently untreatable.
A study conducted at Unicamp and published in Blood magazine shows that the drug used in the chronic treatment of the disease can also provide relief for acute occlusive vessels, which are currently untreatable.
By Karina Toledo
Agência FAPESP – In an article published in Blood magazine, researchers from the Hemocenter at Universidade Estadual de Campinas (Unicamp) showed that hydroxyurea – a drug used in the chronic treatment of sickle anemia – can also help to alleviate symptoms of the acute stage of the disease, which is currently untreatable.
The study, conducted by doctoral student and FAPESP fellow Camila Bononi Almeida, received special mention in the magazine’s editorial section, which is considered the most important in the hematology field.
“A patient arriving at a hospital today with a sickle cell crisis typical of the acute stages of the disease receives only painkillers and hydration. The idea of using hydroxyurea – which is already approved for the chronic treatment of these patients – in the acute stage is very attractive to clinicians. To date, no one had considered it,” comments Nicola Amanda Conran Zorzetto, mentor for the study.
Sickle cell anemia is a hereditary disease characterized by a genetic alteration in hemoglobin, the protein that gives the reddish hue to blood and helps to transport oxygen through the circulatory system.
This change makes the red blood cells take the shape of a sickle or a crescent moon after oxygen is released. The deformed cells become rigid and polymerize, or rather, form groups that adhere to the endothelium and make blood circulation difficult.
“This process is known as vascular occlusion, and we now know that it is related to an inflammatory state resulting from the disease. White blood cells and plaque also adhere to the endothelium, obstructing small vessels,” explains Conran.
In addition to intense pain crises, which often require patients to be hospitalized, the vascular occlusion can cause strokes or lesions to several organs. “Problems such as ulcers, osteonecrosis, pulmonary hypertension and stroke are common,” said the researcher.
In previous studies, Unicamp’s Blood Center, which is managed by the president of the university, Fernando Ferreira Costa, had already shown the benefit of hydroxyurea in the chronic treatment of sickle cell.
“The drug increases the production of another type of hemoglobin, known as fetal hemoglobin. It has this name because normally, it is produced during in utero gestation,” explains Conran.
Fetal hemoglobin is capable of diminishing the polymerization of genetically altered hemoglobin, reducing the risk of vascular occlusion. “However, because this increase in fetal hemoglobin requires months to become effective, no one had considered using the drug in acute crises,” she said.
During her doctorate, Almeida found that as the data in the scientific literature suggest, hydroxyurea has other interesting effects.
“It activates a nitric oxide-dependent cell signaling channel that facilitates vasodilation and hampers the interaction between white and red blood cells and, consequently, their adhesion to the endothelium,” she explains.
In experiments conducted in mouse carriers of sickle cell anemia, scientists observed that medicine not only reduced the adhesion of cells to the wall of vessels but also reversed the inflammation.
“We tested hydroxyurea alone and in association with a substance called BAY73-6691, which also modulates nitric oxide signaling. One drug potentiates the effect of the other,” affirms Almeida.
Step by step
Animals that were genetically modified to develop the disease were split into four groups and received an inflammatory stimulus to induce vascular occlusion.
The first group received only a placebo. The second was treated with hydroxyurea. The third received only BAY73-6691, and the fourth group received a combination of the two drugs.
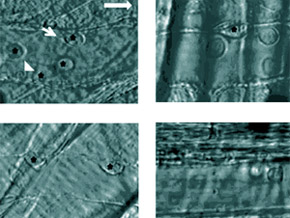
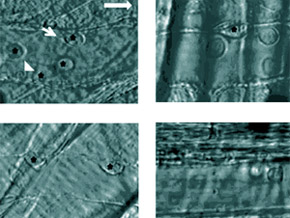
After three hours, the researchers used intravital microscopy – a technique that allows for the observation of blood flow under translucent tissue - to evaluate how the cell interaction and adhesion process works.
In the placebo group, the researchers observed the adhesion of at least six white blood cells every second for every 100 micrometers (μm) of endothelium. In animals that received hydroxyurea or BAY73-6691 separately, this number decreased by 38%. In the group that received the combination of the two drugs, the reduction in cell adhesion was 74%.
In analyzing the interaction of red blood cells with white blood cells that had previously adhered, the scientists found similar results. “This is important because after the white blood cells adhere to the endothelium, the next step of the vascular occlusion process would be the interaction of these cells with circulating red blood cells,” explains Almeida.
The data showed a 44% reduction in the interaction in the group treated only with hydroxyurea and a 62% reduction in the group treated only with BAY73-6691. There was a 69% decrease when the two drugs were combined.
“We also witnessed a significant increase in survival rates in the group that received a combination of hydroxyurea and BAY73-6691 compared to the control group,” explains Almeida.
Prospects
For Conran, although the best results were obtained with a combination of two drugs, hydroxyurea alone also showed significant effects that can be easily applied in clinical practice.
“We are conducting clinical trials with BAY73-6691 drugs for the treatment of Alzheimer disease, and there is interest in testing it in sickle cell anemia. However, hydroxyurea is already available for the treatment of patients,” she said.
However, the researcher stresses that new clinical trials will be necessary to prove the benefits of the medication for the acute stages in humans and determine the correct dosage.
In addition to hydroxyurea, bone marrow transplants are currently the only therapeutic option for sickle cell anemia. The procedure, however, is not recommended for all cases, and a compatible related donor is not always found. “For this reason, everyone is seeking a means to treat the disease and its complications in a more efficient manner,” says Conran.
Almeida’s work received an award at the 16th Congress of European Hematology held in London, England, in 2011. It also received the top prize at the 2010 Congress of the Brazilian Hematology and Hemotherapy Association.
The study is being conducted under the auspices of two other projects funded by FAPESP: one Thematic project, coordinated by Costas, and another Regular Research project, coordinated by Conran. The study also had collaboration from scientists at the Albert Einstein Medical School in New York.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





