

image: MND
The formula developed by a startup supported by FAPESP is used to treat patients without therapeutic possibilities.
The formula developed by a startup supported by FAPESP is used to treat patients without therapeutic possibilities.
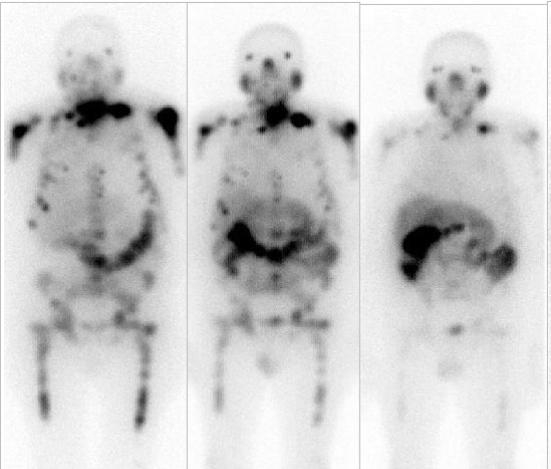
image: MND
By Roseli Andrion | Agência FAPESP – There were 71,730 cases of prostate cancer in Brazil in 2023, according to data from the National Cancer Institute (INCA). Prostate cancer is the most common type of cancer in Brazilian men, accounting for 30% of all cases of cancer among the country’s males. Depending on the stage of the disease, it can greatly affect the quality of the patient’s life.
Researchers at MND Medicina Nuclear based in Campinas, São Paulo state, Brazil, set out to create a local version of a specific radiopharmaceutical for the treatment of prostate cancer. The project is supported by FAPESP’s Innovative Research in Small Business Program (PIPE).
Studies began in 2017 with the aim of developing an indigenous formulation for prostate-specific membrane antigen (PSMA), a glycoprotein found in prostate tissue and overexpressed in prostate cancer cells. It is used as a target in diagnostic imaging via PET scans and in potential therapeutic strategies.
According to Elba Etchebehere, a nuclear medicine specialist and owner-partner in MND Campinas, no such medication was produced in Brazil at that time. “We decided to develop the molecule because one of the many challenges of nuclear medicine is access for all patients, especially in a country as large as Brazil. Producing the molecule locally is essential for this reason,” she says.
During the development process, the regulatory legislation changed and the researchers had to modify the procedure for handling the substance. The COVID-19 pandemic also occurred during the period.
“The changes to the rules made by ANVISA [Brazil’s national health surveillance agency, responsible for regulating medical drugs, devices and procedures] obliged us to adapt our entire structure for the second phase. Then the pandemic hit,” Etchebehere recalls. “We planned to complete the project in 2021 but had to stop for the duration.”
Excellent results
Once they had surmounted the difficulties imposed by social distancing, the researchers were able to resume the development process. “We managed to do radiolabeling with stability for three days. That was a fantastic achievement. We then began compassionate use in patients and obtained excellent results,” she says, adding that 27 patients have taken the radiopharmaceutical to date and most have benefited from it in terms of quality of life.
“One patient had an advanced tumor that had invaded the bladder and rectum. He had to wear a diaper and was very embarrassed about it. We gave him the medication and he was able to stop wearing the diaper two weeks after that. The first dose improved his quality of life. He says the treatment gave him his dignity back,” she recalls.
Although PSMA is now produced by MND, the radioactive component still has to be imported because the lutetium-177 isotope is not produced in Brazil. The importation process is complicated by obstacles relating to release by regulatory bodies on arrival at the airport. “There have been times when it arrived on a Sunday and we were only able to treat patients the following week because of the long delay in releasing it, even when it had been preapproved in the country of origin. Dealing with all this hassle has been very difficult,” she says.
Despite the need to import lutetium-177, the partial reduction in dependence on foreign suppliers is essential to the capacity to provide treatment for Brazilian patients. “When the multipurpose reactor is up and running, Brazil will become independent in this respect. It will also lower costs and create jobs in the segment. Right now, however, the isotope still has to be imported,” she says.
MND’s research has so far reduced the cost of the medication by more than 50%. Although this is a significant difference, it is not yet available for free or at a subsidized price from the SUS, Brazil’s national health service. According to Etchebehere, the treatment does not reach even 0.5% of prostate cancer patients in Brazil despite the cost reduction. If those treated with imports are included, the figure is higher but still less than 1%.
With low toxicity, the treatment can benefit many prostate cancer patients. “It’s hard to know they could lead better lives but lack access to it. Whatever we can do to lower the cost is the best way forward,” she says.
Besides improving the quality of life for these patients, use of the radiopharmaceutical extends survival. “Randomized trials have shown that use of radiolabeled PSMA – not ours but generally speaking – extends survival to 15 months, compared with 11 months for patients not given the treatment,” she says.
Use in other stages
In parallel, studies have also been conducted to find out whether use of the medication in other stages of the disease is also beneficial, rather than limiting its use to compassionate programs. For example, trials have been conducted to assess the concomitant use of substances or even inclusion of radiolabeled PSMA prior to treatment in order to improve the patient’s condition.
PSMA can also be associated with a different radioactive isotope instead of lutetium-177 to treat other types of cancer. “We’re participating in a second project on the use of this molecule. In nuclear medicine we have what’s known as theranostics [a portmanteau of therapeutics and diagnostics], using a radioactive drug [such as PSMA, for example] to diagnose the cancer and a radioactive isotope drug to deliver therapy,” Etchebehere explains. This entails using the molecule with an isotope to locate the tumor and then swap out the isotope to apply the substance as treatment. This project is carried out in partnership with the Cancer Theranostics Innovation Center (CancerThera), a Research, Innovation and Dissemination Center (RIDC) supported by FAPESP.
The approach can be termed personalized medicine insofar as different patients are treated differently since what works well for one may not be so effective for another. “In this project, we’re aiming to use the molecule to treat other tumors. The study involves the State University of Campinas [UNICAMP], the São Paulo Santa Casa charity hospital, and the University of São Paulo [USP] in São Carlos. The novel molecules will be used by UNICAMP’s team of oncologists,” she says.
FAPESP’s support has been essential to the development of the radiopharmaceutical, she stresses. The researchers are to seek permission from ANVISA to import lutetium-177 directly for routine treatment of patients. “We don’t plan to sell the product at this time. We want to focus on offering treatment for patients within our reach. If we can import the isotope with ANVISA’s approval, we have the wherewithal to do that,” she says.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





