

In tests performed in Brazil on mice, one substance promoted 100% survival in association with benznidazole, the antitrypanosomal drug of reference (image: Mae Melvin-CDC)
In tests performed in Brazil on mice, one substance promoted 100% survival in association with benznidazole, the antitrypanosomal drug of reference
In tests performed in Brazil on mice, one substance promoted 100% survival in association with benznidazole, the antitrypanosomal drug of reference
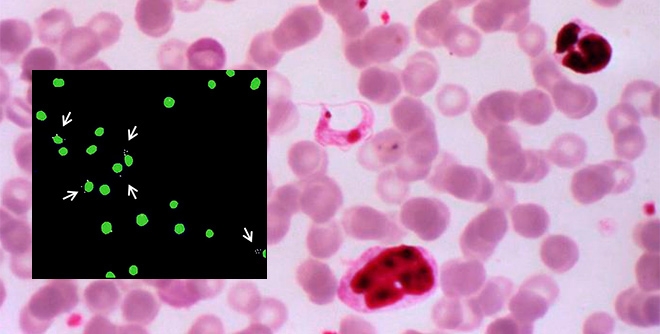
In tests performed in Brazil on mice, one substance promoted 100% survival in association with benznidazole, the antitrypanosomal drug of reference (image: Mae Melvin-CDC)
By Karina Toledo | Agência FAPESP – Three new chemical compounds synthesized by scientists at the University of São Paulo (USP) in São Carlos, Brazil, have been successfully tested on mice for the treatment of the acute phase of Chagas disease. Preliminary tests in the chronic phase have also had positive results.
The three substances have in common the capacity to inhibit the activity of cruzipain, an enzyme essential to the survival of Trypanosoma cruzi, the parasite that causes Chagas disease, in all stages of its lifecycle.
When the researchers tested these compounds in association with the antitrypanosomal drug of reference, benznidazole, they achieved a survival rate of 60%-100%, compared with only 10% when benznidazole was administered alone in the acute phase.
“We’re now embarking on pharmacokinetics studies, which will help us understand how the substances are metabolized in the organism and determine the ideal dose and administration regime. This information will guide the studies designed to lead to progress in preclinical trials,” said Carlos Alberto Montanari, leader of the Medicinal Chemistry Group at USP’s São Carlos Chemistry Institute (IQSC-USP).
The research led by Montanari has been supported by FAPESP since 2005 under the aegis of a program dedicated to drug discovery and development. Since 2014, the group has been funded by the Thematic Project “Molecular design, synthesis and trypanocidal activity of cruzain reversible covalent inhibitors”.
The multidisciplinary research group also includes Andrei Leitão (IQSC-USP), Sérgio de Albuquerque (affiliated with USP’s School of Pharmaceutical Sciences), Antonio Burtoloso (IQSC-USP), Carolina Borsoi Moraes (Federal University of São Paulo) and Lúcio Freitas Júnior (USP’s Biomedical Science Institute).
“It all began with the discovery of a biomacromolecular target, cruzipain, an enzyme that does two important jobs. It helps the parasite recognize, adhere to and invade the host cell. After this process, it has a second effect, which consists of digesting the host cell’s proteins,” Montanari told Agência FAPESP.
Initially, the group at IQSC-USP focused on developing a recombinant version of cruzipain called cruzain. For this purpose, the scientists genetically modified bacteria of the species Escherichia coli to express large amounts of cruzain in laboratory-grown cells.
They were then able to start looking for chemical compounds that inhibited the activity of cruzain and to perform the first tests of interaction between the molecules.
“We performed a virtual analysis of more than 100 million chemical substances in different molecule libraries from various parts of the world. This was possible only thanks to artificial intelligence tools of the machine learning type, capable of analyzing a large amount of data by chemoinformatics to find patterns of molecular recognition that could serve as a basis for predictions,” Montanari said.
Equipped with computational tools and previously obtained information on the three-dimensional structures of the molecules, the researchers selected the most promising substances to interact with cruzain and inhibit its biological function by means of a process known as molecular docking, which predicts the predominant binding mode in the complex formed with the enzyme as well as its inhibitory potential.
After this initial screening, 250 small chemical compounds were selected and synthesized by the group at IQSC-USP over a period of several years for in vitro interaction trials.
“We used the information obtained from the machine learning tools in conjunction with data on the 3D structure of cruzain obtained by X-ray crystallography,” Montanari explained. “Thanks to a combination of these datasets, the structure of the molecule to be synthesized could be ‘learned by heart’ to increase the chances of success in inhibiting the enzyme.”
The synthesized compounds were first tested in vitro against the recombinant enzyme with the aim of proving that they did in fact work according to the interaction mechanism studied by the researchers. The most successful candidates were then tested directly against the parasite, also in vitro.
Approximately six of the 250 initially screened compounds were tested in animals. According to Montanari, only those found to be effective at very low levels were chosen for continued testing at the in vivo trial stage.
“In practice, our synthesis of molecules follows the concept of hypothesis-based planning,” he said. “This means that after the in vitro biochemical testing of a compound, we use the results to plan and refine the next molecule to be synthesized. More recently, we succeeded in leveraging prior results to approach the ideal molecular structure and selected 12 chemical substances with the potential for preclinical development. Testing in humans will be the next stage.”
In vivo trials
The first compound tested alone in rodents did not prove very effective in terms of promoting survival, so the scientists decided to proceed with the trials by combining cruzain inhibitors with benznidazole, the standard drug for the treatment of Chagas disease.
“Although benznidazole works well in the acute phase, it isn’t very effective against the parasite during the chronic phase, which may manifest many years after the patient was infected by T. cruzi,” Montanari said. “In addition, it’s highly toxic and has many adverse side effects. Combined therapy would enable us to lower the dose and mitigate the side effects.”
Once the acute phase is over, he explained, the parasite may remain silent for years in the human organism without causing symptoms or being detected in laboratory tests. A medical diagnosis is possible only when chronic-phase complications arise, such as enlargement of the ventricles of the heart (which affects some 30% of patients and typically leads to heart failure), dilatation of the esophagus, and enlargement of the colon (which affects up to 10% of patients and can lead to impairment of peristalsis and sphincter insufficiency).
“We plan to test our drug candidates in the chronic phase, when the parasite can again be detected in the organism,” Montanari said. “Today, there are no effective therapeutic options for the chronic phase. That’s why we had the idea of combined therapy.”
The tests were performed on mice infected with the Y strain of the parasite, which is one of the most virulent strains found in Brazil. According to Montanari, the compounds synthesized by his group displayed a strong synergistic effect when combined with benznidazole.
“We applied an innovative concept that’s much used by the FDA [Food and Drug Administration, the US health protection agency] and entails administering a subtherapeutic dose in the hope that the adverse effects of isolated substances will be minimized,” he said. “Apparently it worked, since none of the mice died and we observed no adverse effects.”
For three of the six compounds tested in animals, the researchers have established the ideal dose ratio for the two substances (benznidazole and cruzain inhibitor). All three belong to a chemical class known as mimetic peptides, meaning they have similar physicochemical properties to those of peptides, although their chemical structure is not peptidic. As a result, they are not digested by stomach enzymes and can be administered by mouth, as well as being more chemically stable in general.
“They’re performing well in chronic phase treatment in rodents,” Montanari said. “Once the pharmacokinetics trials are completed, we’ll start work on refining the administration regime and dose. Next, we plan to seek partners in the pharmaceutical industry on the basis of a public-private partnership model. After the preclinical trials, the process becomes very costly, and no public university has the resources or funds to go it alone.”
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





