

Team at the Molecular and Cellular Biology Laboratory of the Unifesp Hemotherapy Center presented findings of studies conducted over the past 15 years during FAPESP Week Michigan-Ohio (image: Angela Eugênio e Marimélia Porcionatto/Unifesp and Bryan Strauss/Icesp)
Brazilian team presented findings of studies conducted over the past 15 years during FAPESP Week Michigan-Ohio.
Brazilian team presented findings of studies conducted over the past 15 years during FAPESP Week Michigan-Ohio.
Team at the Molecular and Cellular Biology Laboratory of the Unifesp Hemotherapy Center presented findings of studies conducted over the past 15 years during FAPESP Week Michigan-Ohio (image: Angela Eugênio e Marimélia Porcionatto/Unifesp and Bryan Strauss/Icesp)
By Karina Toledo, in Ohio | Agência FAPESP – The search for new therapeutic targets for what are known as lymphoproliferative disorders, a group of disorders that includes neoplasias such as leukemia, lymphoma and myeloma, has been the focus of the Molecular and Cellular Biology Laboratory in the Hematology and Hemotherapy Division, Department of Clinical and Experimental Oncology at the Federal University of São Paulo (Unifesp).
The group’s coordinator, Professor Gisele Wally Braga Colleoni, presented advances in identification of biomarkers associated with multiple myeloma, in Columbus, Ohio on the final day of FAPESP Week Michigan-Ohio. The symposium was held March 28 – April 1 for the purpose of promoting increased cooperation between scientists from São Paulo and the United States.
"Multiple myeloma is still an incurable disease. Despite advances in the use of immunomodulatory drugs, proteasome inhibitors [important pathways for degradation of proteins inside cells] and autologous bone marrow transplants, the disease, at some point, ends up recurring. The five-year survival rate after diagnosis is currently only 35%. So there is still a lot of progress that needs to be made before we understanding its mechanisms and how to treat it,” said Colleoni in an interview with Agência FAPESP.
As explained by the researcher, the disease is characterized by the uncontrolled proliferation of a type of immune system cell known as a plasma cell, derived from B-lymphocytes and responsible for producing antibodies (proteins like immunoglobulin, responsible for humoral immunity). These cases account for 1% of all cancers and 10% of the hematologic neoplasias.
"When the malignant proliferation of plasma cells occurs in a localized manner, usually in the bones or facial sinuses, it is called plasmacytoma. When it occurs in systemic form, it is classified as multiple myeloma,” Colleoni explained.
In more advanced cases, the level of bone marrow plasma cell infiltrates increases considerably and begins to occupy the space of the other blood products, compromising system functioning. The most common symptoms are bone pain, infections, anemia and kidney failure.
The Unifesp group began its search for biomarkers of multiple myeloma 15 years ago when it became a member of the task force of the Clinical Cancer Genome Project, led by Marco Antonio Zago, then professor and currently president of the University of São Paulo (USP). The study is currently funded by FAPESP through the thematic project entitled, "Identification of biomarkers and possible therapeutical targets in B-cell lymphoproliferative disorders".
"From 2000 to 2008, we received funding from FAPESP to collect and store samples of bone marrow and serum from all multiple myeloma patients in treatment at the Hospital São Paulo at Unifesp. Ever since, we have continued to collect and analyze this material and compare it with normal cells for the purpose of identifying genes and important pathways for cellular functions that are differentially expressed in tumors," Colleoni said.
The group observed that in 90% of the samples of multiple myeloma, there was increased expression of the TRIAP1 gene, an inhibitor of apoptosis (programmed cell death) that quite possibly helps tumor cells survive and thus represents a potential therapeutic target. In tests conducted in vitro, silencing the TRIAP1 gene induced the death of a large percentage of the tumor cells.
"We have still not been able to conduct in vivo tests because there is no pharmacological inhibitor for the TRIAP1 gene, and when we silence the gene in cell culture, the cells die before we are able to obtain a sufficient number to implant in animal models in order to induce tumor formation,” Colleoni explained.
The group then decided to utilize a murine model to test pharmacological inhibition of the HSP70 gene, which provides support to the TRIAP1 gene and in this way, also helps tumor cells survive. According to Colleoni, the HSP70 gene is usually hyperexpressed in several types of cancer, including myeloma. The therapy was tested together with a proteasome inhibitor known as bortezomib.
"We achieved good results with the HSP70 gene inhibitor in vitro, but in the animal model, we have not yet been able to reduce the size of the tumor in an efficient manner, unrelated to the isolated or associated use of bortezomib. We are currently adjusting the model," Colleoni said.
Other research fronts
The Unifesp group has also worked on other fronts in searching for therapeutic targets to fight multiple myeloma. One of them involves development of a vaccine designed to stimulate the immune system to recognize and attack tumor cells. According to Colleoni, since it is a disorder that originates in the defense cells, the B cell-mediated immunity (humoral) is often quite compromised.
The group identified proteins that are expressed in a considerable number of the tumor cells, including MAGEC1/CT7 and MAGEA3/6, with high immunogenic potential, in other words, with the capacity to induce immune cell response (mediated by T-lymphocytes). The findings caught the attention of other research groups, among them one led by Kris Thielemans at the Free University of Brussels in Belgium, and another led by Professor Sara Saad at the University of Campinas (Unicamp).
"In this case, we proposed the collection of immature cells from the patient’s own immune system to be treated and sensitized in vitro with the tumor antigens. Once they have matured, these cells will be reused in the patient with the hope that they will attack the tumor cells. Before that however, other treatments have to be used to reduce the tumor burden,” Colleoni said.
Thielemans’ team has used a similar method in experimental treatments of melanoma. Colleoni stresses that this type of vaccine is specific to each patient however.
"It is not a commercial product. Immunotherapy however has been considered the greatest revolution in cancer treatment in the past five years and many significant results have been presented with the inhibition of proteins such as PD-1, PDL1 and CTLA4. This stimulates the T-lymphocytes to recognize the tumor and eliminate it,” the researcher said.
The search for therapeutic targets has also been focused what are known as bone marrow stromal cells. As Colleoni explained, this type of cell is found in every tissue of the body and serves as a support mechanism, producing growth factors, for example.
"Somehow, the tumor is able to reprogram these bone marrow stromal cells so that they begin to work to provide feedback to it. We are looking for a way to interrupt this communication and block the action of these stromal cells in order to help fight the tumor cell,” the researcher said.
Lastly, the team has been dedicated to investigating the existence of tumor stem cells in samples of multiple myeloma. Such cells could constitute an additional possible therapeutic target since they are able to promote the tumor’s recurrence or relapse through conventional treatment.
"We conducted the analysis using a technique known as flow cytometry. We started from the data in the literature, indicating that these cells, if in fact they exist, should be expected to express some markers of pluripotency such as the proteins ALDH+ and CD34+. The studies also indicate that since they are considered myeloma stem cells, they cannot express protein CD138," she explained.
Some of the data presented by Colleoni was published in articles in the journals: Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease; Cancer Immunology, Immunotherapy; Cancer Letters; and Cancer Immunity.
Osteoarthritis
In the same session dedicated to the topic of "Medicine and Health,” Professor Sudha Agarwal of the Biosciences Division at the Ohio State University, presented data from a FAPESP-funded project carried out in partnership with Mario Ferreti Filho, a professor from the Department of Orthopedics and Traumatology at Unifesp.
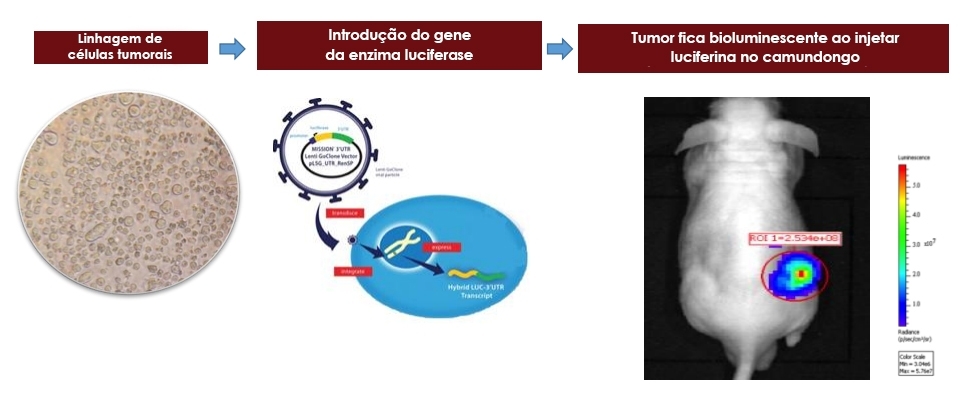
The goal of the study was to understand the mechanism through which performance of moderate physical exercise improved inflammation in the cartilage of carriers of osteoarthritis. Through experiments with bioluminescent mice, the group showed that training modulates the expression of several genes and alters the balance of inflammatory and anti-inflammatory molecules in the body, improving inflammation in a systemic manner.
The researchers are currently trying to identify biomarkers that are able to indicate to what extent the patient is responding to the therapeutic interventions.
Also taking part in the Friday afternoon panel was researcher David Symer, associated with the Ohio State University Comprehensive Cancer Center, and University of São Paulo Medical School (FMUSP) Professors Marta Imamura and Linamara Battistella.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





