

A study performed at the University of São Paulo shows that cellular immunity is just as important as the production of antibodies, if not more so, for the control of dengue virus infection (image: Wikimedia Commons)
A study performed at the University of São Paulo shows that cellular immunity is just as important as the production of antibodies, if not more so, for the control of dengue virus infection.
A study performed at the University of São Paulo shows that cellular immunity is just as important as the production of antibodies, if not more so, for the control of dengue virus infection.
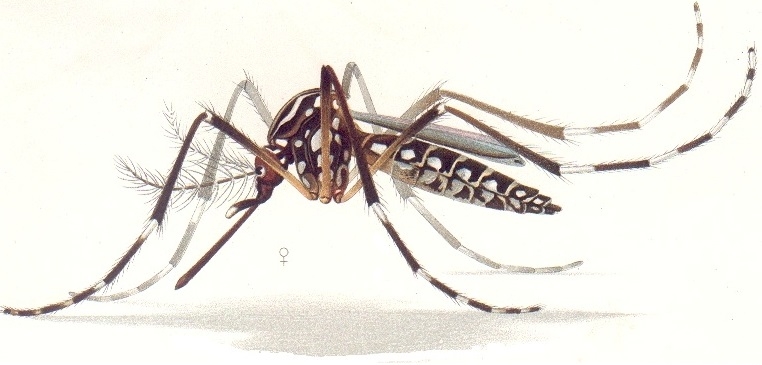
A study performed at the University of São Paulo shows that cellular immunity is just as important as the production of antibodies, if not more so, for the control of dengue virus infection (image: Wikimedia Commons)
By Karina Toledo | Agência FAPESP – A Brazilian study published in the journal Virology shows that cellular immunity mediated by T lymphocytes is as important as antibody-mediated immunity, if not more so, for the control of dengue virus infection.
According to the authors, this new evidence may be significant in the process of choosing the ideal vaccine for public immunization programs.
Any viral infection stimulates two types of immune response in humans, explained Luís Carlos de Souza Ferreira, Head of the Vaccine Development Laboratory at the Microbiology Department of the University of São Paulo’s Biomedical Science Institute (ICB-USP): the production of specific antibodies that recognize structures on the surface of the virus, and the activation of cytotoxic T lymphocytes (CD4 and, above all, CD8) that recognize and destroy the organism’s own infected cells.
Sanofi Pasteur developed its dengue vaccine, which is now available, using modified yellow fever virus. It is capable of inducing the production of antibodies against dengue virus, but the cellular immunity it induces is against the yellow fever vaccine virus.
“Sanofi’s vaccine uses what we call a chimeric virus,” Ferreira explained. “They placed dengue virus structures in the envelope, but the core is yellow fever virus. The issue is that cytotoxic lymphocytes preferentially recognize proteins expressed by the virus only during its multiplication inside the infected cell but not present in the viral particle.”
The vaccine being developed by Brazil’s Butantan Institute, which has just received permission from ANVISA, the National Public Health Surveillance Agency, to proceed to Phase III clinical trials, uses attenuated dengue virus and therefore induces both types of immune responses against dengue.
“Brazil is currently hesitating between adopting Sanofi’s vaccine or waiting for Butantan Institute to complete clinical trials of the vaccine developed here. However, only the Brazilian vaccine, developed in partnership with the US National Institutes of Health, can induce cellular immunity against dengue, which is crucially important, as we show,” Ferreira said.
Methodology
The experiments described in the Virology paper were conducted using an animal model during Jaime Henrique Amorim’s postdoctoral research with support from FAPESP and in partnership with the University of São Paulo’s Tropical Medicine Institute (IMT-USP).
The researchers first inoculated mice intracranially with ACS46, a strain of dengue virus type 2 (DENV-2) that induced an immune response without making the animals sick.
After this “immunization” procedure, they challenged the same group of mice with JHA1, a more aggressive isolate from DENV2 that can be lethal even in small doses. Nevertheless, all the mice survived thanks to the protection acquired from prior exposure to the virus.
“This method of intracranial inoculation is used by laboratories worldwide in viral propagation models,” Ferreira said.
The next step comprised isolating the antibodies produced in response to the non-lethal strain of the virus and transferring them to the other group of animals that had not been contaminated with DENV2.
“We performed this procedure until the level of antibodies in the blood of non-infected mice was equivalent to the level in the group exposed to ACS46. Then we challenged them with the aggressive isolate from DENV2, and they all died,” Ferreira said.
In a second experiment, the researchers destroyed the CD4+ and CD8+ T lymphocytes produced by the group of mice exposed to the non-lethal strain of DENV2 using specific antibodies against these defense cells. The animals were then challenged with the aggressive strain, and practically all of them died.
“This result led us to conclude that at least in this experimental model, the response mediated by T lymphocytes is just as important as immunity mediated by antibodies, if not more so. This suggests that Butantan Institute’s vaccine will protect human subjects more effectively,” Ferreira said.
Phase III trials of the Butantan Institute’s dengue vaccine will involve 17,000 volunteers in three age groups: children aged 2-6 years, children and adolescents aged 7-17 years, and adults aged 18-59 years. The goal is to demonstrate that the vaccine assures effective protection against all four subtypes of the dengue virus. The first phase of the project was funded by FAPESP.
The article “Antibodies are not required for a protective immune response against dengue virus elicited in a mouse encephalitis model” (doi: 10.1016/j.virol.2015.10.006) can be read at www.sciencedirect.com/science/article/pii/S004268221500433X.
Other side
According to a press release issued by Sanofi Pasteur, its vaccine “induces a cellular and humoral response leading to the formation of serotype-specific antibodies, as demonstrated in a scientific study that evaluated the vaccine in humans and has recently been published by the highly respected scientific journal Nature”.
The Virology study was “experimental, performed in animals, and its findings cannot be extrapolated to form conclusions about efficacy in humans,” according to the release issued by the vaccines division of the multinational pharmaceutical company Sanofi.
“It is important to stress that studies of efficacy in humans, which are mandatory to register a dengue vaccine, have been performed only by Sanofi Pasteur. A cellular response may contribute to an enhanced response to the disease but does not prevent infection, which is the role of antibodies, and these must be specific. Sanofi Pasteur has demonstrated the presence of specific antibodies against dengue virus and the quality of these antibodies via definitive serotype-specific responses,” the release said.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





