

Capsules that are a few nanometers in diameter can successfully deliver drugs to the brain and combat glioblastoma (image: Wikimedia Commons)
Capsules that are a few nanometers in diameter can successfully deliver drugs to the brain and combat glioblastoma.
Capsules that are a few nanometers in diameter can successfully deliver drugs to the brain and combat glioblastoma.
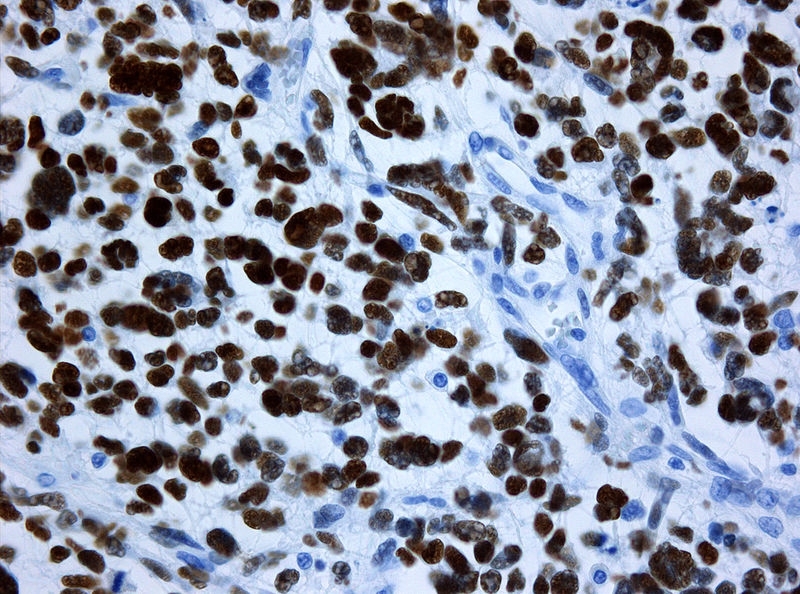
Capsules that are a few nanometers in diameter can successfully deliver drugs to the brain and combat glioblastoma (image: Wikimedia Commons)
By Diego Freire | Agência FAPESP – Drugs designed to treat brain diseases must cross the blood-brain barrier, a selectively permeable mass of tightly packed cells that protects the central nervous system from potentially neurotoxic substances in the blood. According to experts, 98% of drugs are unable to cross the blood-brain barrier, and those that can do so must typically be administered in high doses that can have potentially harmful side effects.
To enhance penetrability and use safer doses, researchers at the University of São Paulo’s School of Pharmaceutical Sciences (FCF-USP) in Brazil used capsules that are a few nanometers in diameter, and are capable of crossing the blood-brain barrier and delivering a drug to target cells – in this research project, parts of the brain were invaded by glioblastoma, the most common type of malignant brain tumor in adults and a condition for which no effective pharmacological treatment exists.
Tests in mice with glioblastoma showed that nanocapsules containing indomethacin crossed the blood-brain barrier and reduced tumor volume by 70%. These results were obtained during the project “Study of the therapeutic efficacy of indomethacin and ethyl ester indomethacin nanocapsules: intravital microscopy assays”, which was supported by FAPESP and was led by Sandra Helena Poliselli Farsky, the principal investigator.
“One of the adverse side effects of indomethacin is gastrointestinal injury. In our experiments, chronic oral administration of a non-encapsulated formulation of this anti-inflammatory drug caused the animals to die as a result of gastrointestinal injuries,” Farsky said. “In contrast, administration of nanocapsules loaded with indomethacin didn’t cause gastrointestinal damage and significantly reduced tumor volume.”
According to Stephen Fernandes de Paula Rodrigues, a postdoctoral researcher supervised by Farsky, “the success of these tests represents a major opportunity for improvements in the health of patients with glioblastoma, which is, in most cases, associated with short survival times, usually of about 12 months. It’s a severe disease, and the available treatments are not very effective. Surgery can’t remove all the tumor cells because they infiltrate normal brain tissue. Chemotherapy must be highly aggressive in order to cross the blood-brain barrier and has significant adverse side effects.”
Conventional chemotherapy for glioblastoma entails administration of temozolomide, an expensive drug with no guarantee of efficacy. One of the adverse side effects of its administration at concentrations high enough to cross the blood-brain barrier is damage to the red bone marrow, which contains the hematopoietic stem cells that produce blood cells and immune cells. Another adverse side effect is leukopenia, a low white blood cell count that increases susceptibility to infection.
The lipid-core nanocapsules used as an alternative to conventional chemotherapy in Farsky’s study were developed by Sílvia Stanisçuaski Guterres and Adriana Raffin Pohlmann, researchers who are affiliated with the Federal University of Rio Grande do Sul (UFRGS). As a polymer wall, they used poly-epsilon-caprolactone, a biodegradable, biocompatible, non-toxic compound. Indomethacin was added to the nanocapsules to control inflammation, reduce pain and combat fever.
The nanocapsules were labeled with a fluorescent dye during synthesis and were tracked in the bloodstream and brain tissue using intravital microscopy, a high-resolution real-time in vivo observation and imaging technology.
Fluorescence would normally have been observed only inside the blood vessels, as the blood-brain barrier would prevent molecules from entering the brain tissue, but with the nanocapsules, the fluorescence was tracked from blood vessels to the functional tissue of the brain, showing that the drug had successfully crossed the blood-brain barrier.
Next, the researchers induced glioblastoma in mice and treated them with the indomethacin-loaded nanocapsules. Tumor volume was found to decrease without adverse side effects, suggesting successful transport of indomethacin and confirming the drug’s efficacy in tumor suppression.
The researchers consider the results promising, saying that they could lead to the development of a new strategy for the treatment of glioblastoma and other diseases that affect the central nervous system, such as Alzheimer’s and Parkinson’s.
“The blood-brain barrier is an obstacle to the administration of several drugs, so the use of nanocapsules to ‘carry’ drugs and enable them to easily permeate the barrier is a significant advance. It might even be possible to deploy this technique to prevent disease in healthy areas of the brain.”
The research findings are described in the article “Lipid-core nanocapsules act as a drug shuttle through the blood-brain barrier and reduce glioblastoma after intravenous or oral administration”, published in the Journal of Biomedical Nanotechnology. The authors are Stephen Fernandes de Paula Rodrigues, Luana Almeida Fiel Baumbach, Ana Lucia Borges Shimada, Natalia Pereira, Sílvia Stanisçuaski Guterres, Adriana Raffin Pohlmann and Sandra Helena Poliselli Farsky.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





