

Genetic profiles of microorganisms isolated from patients with urinary tract infection display a high degree of resistance and virulence. The superbug KPC was found in samples (bacteria with virulence phenotype known as hypermucoviscosity / photo: André Pitondo Silva)
Genetic profiles of microorganisms isolated from patients with urinary tract infection display a high degree of resistance and virulence. The superbug KPC was found in samples.
Genetic profiles of microorganisms isolated from patients with urinary tract infection display a high degree of resistance and virulence. The superbug KPC was found in samples.
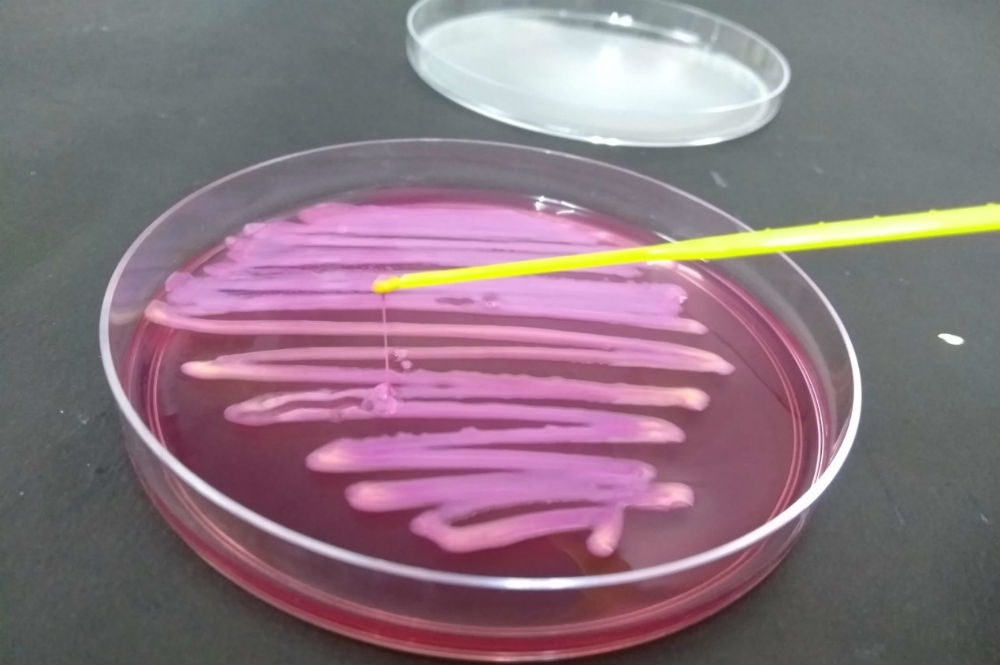
Genetic profiles of microorganisms isolated from patients with urinary tract infection display a high degree of resistance and virulence. The superbug KPC was found in samples (bacteria with virulence phenotype known as hypermucoviscosity / photo: André Pitondo Silva)
Karina Toledo | Agência FAPESP – The bacterium Klebsiella pneumoniae is one of the most frequent causes of hospital-acquired (nosocomial) infections and is also one of the most drug-resistant bacteria.
Carbapenemase-producing K. pneumoniae (KPC) is a well-known superbug, so-called because it is resistant to almost all antibiotics. Carbapenemase is an enzyme that can inactivate carbapenems, the most powerful drugs available for the treatment of severe infection.
A recent study supported by FAPESP and published in the Journal of Global Antimicrobial Resistance shows that KPC and other multidrug-resistant bacteria are spreading outside hospitals.
When the researchers analyzed K. pneumoniae specimens isolated from 48 outpatients diagnosed with urinary tract infections in the Ribeirão Preto region of São Paulo state, they found that 29 (60.4%) patient specimens contained bacteria considered to be multidrug-resistant because they are not susceptible to three or more antibiotic classes. Seventy-three different virulence genes were detected in 30 (62.5%) specimens. Virulence genes encode proteins that enable the pathogen to evade the host’s immune system or spread easily in the environment.
“We were surprised to find bacteria with such extensive multiresistance and virulence in people who weren’t in the hospital. Some of the bacteria analyzed had a genetic profile typical of the strains that cause hospital-acquired infections,” André Pitondo da Silva, a professor at the University of Ribeirão Preto (UNAERP) and a coauthor of the article, told Agência FAPESP.
Pitondo-Silva was the principal investigator of a project that compared the molecular profiles of Klebsiella specimens isolated from hospital patients in five Brazilian cities, one in each region of the country (Londrina in the south, Brasília in the center-west, Teresina in the northeast and Manaus in the north, as well as Ribeirão Preto, representing the southeast) and five countries representing other continents (New Zealand, Canada, the Netherlands, South Africa and India).
The study began when Pitondo-Silva was a researcher at the University of São Paulo’s Ribeirão Preto School of Pharmaceutical Sciences (FCFRP-USP). Samples from the Ribeirão Preto community were obtained by chance. The researchers collected bacterial isolates from patients at a local hospital. “Attached to this hospital was a private clinical laboratory used by people living in the city and neighboring towns. The lab was also responsible for testing patients at the hospital. When we received samples of K. pneumoniae, we noticed that the patient’s hospital ward or department was not specified in some cases. We interviewed the lab staff about this, and they told us the samples were from people who weren’t hospitalized. Therefore, we decided to study these bacteria in the community and compare them to bacteria from the hospital environment,” Pitondo-Silva explained.
The paper, published in the Journal of Global Antimicrobial Resistance, concerns only the analysis of the 48 samples from nonhospitalized patients, 31.3% of whom were over 60 years old, while 27.1% were aged 30-59, 14.6% were aged 16-29, and 12.5% were aged 1-15. One was a newborn, and six were of unidentified age. Seventy-five percent of the samples analyzed were from women.
Genetic profiling
The scientists first confirmed that the isolates were K. pneumoniae using matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF/MS). Next, they performed an antibiogram to determine the pathogens’ drug resistance and antimicrobial susceptibility profiles.
We cultured the bacteria from each sample in Petri dishes and placed small disks impregnated with antibiotics on top of the cultures,” Pitondo-Silva said. “We simultaneously tested 38 different antibiotics and then evaluated the ability to inhibit microbial growth for each.”
All 48 isolates of K. pneumoniae were found to be nonsusceptible to four or more of the antibiotics tested. All were resistant to trimethoprim, 47 (97.9%) were resistant to sulfonamides, 43 (89.6%) were resistant to nalidixic acid, 40 (83.3%) were resistant to nitrofurantoin, 26 (54.2%) were resistant to trimethoprim/sulfamethoxazole, 24 (50.0%) were resistant to doxycycline, 19 (39.6%) were resistant to minocycline, 18 (37.5%) were resistant to lomefloxacin, 17 (35.4%) were resistant to piperacillin/tazobactam, 16 (33.3%) were resistant to streptomycin and cefaclor, 15 (31.3%) were resistant to ticarcillin/clavulanic acid, 14 (29.2%) were resistant to ceftaroline, 13 (27.1%) were resistant to ampicillin/sulbactam, cefixime and tobramycin, 11 (22.9%) were resistant to amoxicillin/clavulanic acid, cephalothin and norfloxacin, 10 (20.8%) were resistant to chloramphenicol, 9 (18.8%) were resistant to aztreonam, cefazolin, cefepime, ceftriaxone, ertapenem, imipenem and meropenem, 8 (16.7%) were resistant to amikacin, cefotaxime, cefuroxime, ciprofloxacin, ceftazidime, tetracycline and ofloxacin, 7 (14.6%) were resistant to doripenem, cefoxitin and levofloxacin, and 5 (10.4%) were resistant to gentamicin.
Resistance and virulence genes were investigated using PCR (polymerase chain reaction) and sequencing. Genetic relations between the bacteria were analyzed using ERIC-PCR and MLST (multilocus sequence typing). ERIC stands for enterobacterial repetitive intergenic consensus.
“We were surprised by the results,” Pitondo-Silva said. “Seven isolates had genetic profiles compatible with clonal complex 258 [CC258], which is generally associated with hospital-acquired infections and spreads very rapidly. We also found several KPC-producing bacteria.” CC258 is the most widespread carbapenem-resistant group of K. pneumoniae.
Two other isolates displayed hypermucoviscosity, a virulence phenotype found only in hospitals. Hypermucoviscous bacteria produce a thick, viscous biofilm that adheres to the bladder epithelium and is hard to eliminate.
“There were no clinical records for the cases studied, so we knew nothing about these persons’ medical histories or health. Our hypothesis is that they were hospitalized in the past and colonized by these multidrug-resistant bacteria while in the hospital,” Pitondo-Silva said.
Opportunism
K. pneumoniae is considered an opportunistic bacterium because it can remain part of a person’s microbiota for years without causing problems but may suddenly produce symptoms if immunity is weakened by sickness, therapy or aging. The symptoms range from lung and urinary tract infections to wound infection and even sepsis (generalized infection).
“Patients with a recurrent urinary tract infection risk developing pyelonephritis [inflammation of the kidney, typically due to a bacterial infection], which can lead to kidney failure and even sepsis. These patients may pass on these multidrug-resistant microorganisms when they are readmitted to the hospital,” Pitondo-Silva said.
The main form of contamination is contact with body fluids from an infected patient, which can happen when improperly sterilized catheters are used, for example. “When hospitals identify superbugs, especially KPC-producing multidrug-resistant bacteria, they have strict protocols to prevent dissemination and may even ban patient visits,” Pitondo-Silva said.
Knowledge of the molecular characteristics of the bacteria found in hospitals in Brazil’s different regions helps understand how resistance and virulence genes are spreading and how the species are is evolving. This information is essential to control infections and treat patients correctly.
“It’s very important to determine which antibiotics bacteria are susceptible to. Prescribing the wrong drug could make the patient’s condition worse by selecting for a more resistant strain,” Pitondo-Silva said.
At a hospital in Londrina, Paraná, the same researchers found specimens of K. pneumoniae resistant to all currently available antibiotics (pandrug-resistant). Their findings were published in the journal Infection, Genetics and Evolution in 2017. In such cases, clinicians typically prescribe two or more drugs to try to eliminate the pathogen through synergistic drug action.
In addition to bacteria isolated from community- and hospital-acquired infections, the group is currently studying the resistance and virulence profiles of oral Klebsiella infections and the possible dissemination of multidrug-resistant bacteria in the environment via rivers and hospital wastewater.
The article “Molecular characterization of multidrug-resistant Klebsiella pneumoniae belonging to CC258 isolated from outpatients with urinary tract infection in Brazil” by Paola Aparecida Alves Azevedo, João Pedro Rueda Furlan, Guilherme Bartolomeu Gonçalves, Carolina Nogueira Gomes, Rafael da Silva Goulart, Eliana Guedes Stehling and André Pitondo-Silva can be retrieved from: www.sciencedirect.com/science/article/abs/pii/S2213716519300323?via%3Dihub.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





