
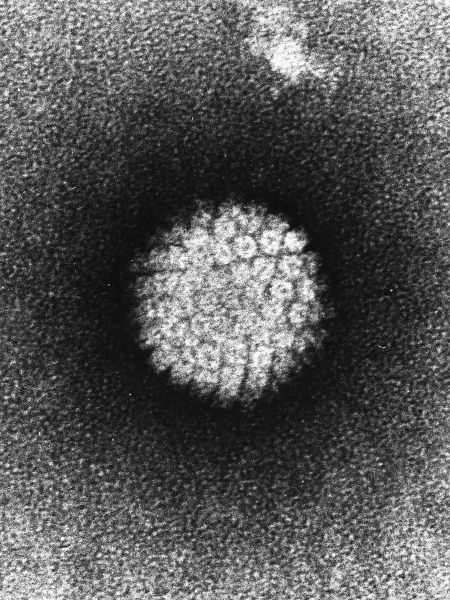
Study collected five years of data on 3,000 men in Brazil, Mexico and the United States. Precancerous lesions took two years to appear in some cases (image: Wikimedia Commons)
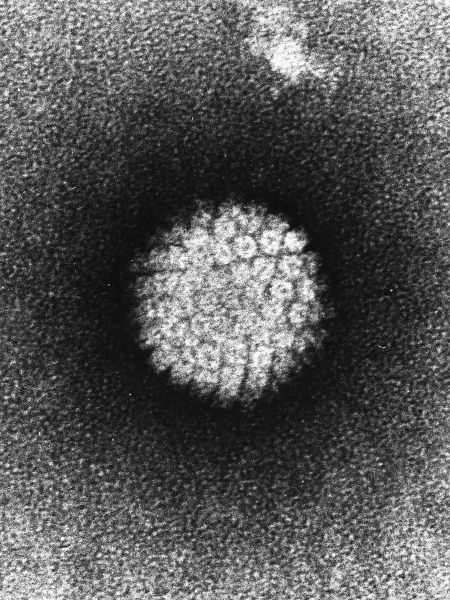
Study collected five years of data on 3,000 men in Brazil, Mexico and the United States. Precancerous lesions took two years to appear in some cases.
Study collected five years of data on 3,000 men in Brazil, Mexico and the United States. Precancerous lesions took two years to appear in some cases.
Study collected five years of data on 3,000 men in Brazil, Mexico and the United States. Precancerous lesions took two years to appear in some cases (image: Wikimedia Commons)
By Ricardo Zorzetto | Pesquisa FAPESP magazine – In January 2017, the Brazilian public health system began vaccinating boys aged 12 and 13 against human papillomavirus (HPV). By early June, however, only 595,000 (16.5% of this age group) had received the first of two doses of the imported vaccine that affords protection against four types of HPV.
Transmitted by direct contact with infected areas of skin or mucous membranes during sexual intercourse, HPV is associated in men with the development of genital and anal warts, as well as cancers of the penis, anus, mouth and throat. Because the use of a condom does not always prevent transmission of the virus, health experts say that the best way to combat dissemination is by vaccinating the uncontaminated population. At the end of June, the Health Ministry recommended vaccination of boys in a wider age bracket, from 11 to 14. This made the 80% vaccination target by end-2017 more challenging. The vaccine has been available for girls for a longer period, but this proportion of girls has not even been vaccinated.
The first signs that it would be necessary to redouble efforts to protect boys appeared shortly after published studies began to show how and for how long infection by HPV progresses before genital warts and precancerous lesions develop in males. “For some time, HPV has been known to lead to warts and tumors in the male genital region, but there were no studies that measured the probability that infection would lead to lesions or how long it took for this to happen,” said biochemist Luisa Lina Villa, a professor at the University of São Paulo’s Medical School (FM-USP).
Villa was one of the first Brazilian researchers to identify the presence of HPV in penile cancer back in the 1980s, and for almost a decade, she has been coordinating the Brazilian part of the epidemiological study, “HPV infection in men (HIM)”. The HIM Study is funded by the United States National Cancer Institute (NCI), São Paulo Research Foundation – FAPESP, and Merck Sharp & Dohme, the pharmaceutical company that makes the quadrivalent HPV vaccine Gardasil. It began with a five-year survey of the sexual health of 4,100 men aged 18-73 in Brazil, Mexico and the US.
The HIM Study has led to dozens of scientific articles. Three of these papers published between 2015 and 2017 presented a detailed natural history of HPV infection. Two were about the work of epidemiologist Anna Giuliano and her group at the Moffitt Cancer Center in Florida. Giuliano is the principal investigator of the HIM Study. Her group described the results from assessments of 3,000 of these men. At the start of the survey, none of the men had HPV infections or any other sexually transmitted diseases. Over time, some contracted the virus, which was identified by genetic testing of material collected from the penis and scrotum.
Approximately 72% of the Brazilians surveyed were infected by HPV at some point in the survey. This is a significantly higher proportion than men in Mexico (62%) or the US (61%). Four of the 37 types of HPV investigated were found most frequently: two are considered low-risk because they tend to cause warts, but not cancer (HPV6 and HPV11), and two are high-risk (HPV16 and HPV18). The vaccine that is available free of charge from the Brazilian health service is designed to combat types 16 and 18.
One of the assessments used data from 3,033 participants in all three countries. In this case, 1,788 were infected by at least one type of HPV, and 86 (5% of those infected) developed genital warts (condyloma). Only nine of the men with HPV had precancerous lesions, which in these cases, were penile intraepithelial neoplasia (PeIN).
One in four cases of infection by HPV6 or HPV11 led to warts containing the same viruses. The time between infection and the appearance of warts was almost eight months for HPV6 and four months for HPV11. Almost 60% of the precancerous lesions contained the high-risk type HPV16. In most cases, there was a lag of almost two years between infection and the development of PeIN, according to an article published in 2015 in European Urology.
An analysis of the Brazilian data was published this year in the Brazilian Journal of Infectious Diseases. Out of 1,118 participants in São Paulo, 815 had HPV and 35 developed genital lesions. During the survey, 16% of the participants with HPV6 and 16% of those infected by HPV11 developed genital warts within nine and seven months, respectively. This development was slower than those of Mexicans and Americans covered by the survey. In the Brazilian sample, 1% of those with HPV16 developed precancerous lesions within 25 months.
In their conclusions, the authors of the Brazilian study drew attention to the fact that HPV types 6, 11, 16 and 18, which the quadrivalent vaccine is designed to combat, were found in 80% of the warts and precancerous lesions. They also recommend a broader policy of vaccination for boys, since men continue to be infected by the virus during their lives and transmit it to partners of both sexes. In one of the HIM Study articles, the researchers pointed to the successful case of Australia, the first country to implement a national program of immunization against HPV. More than 80% of Australia’s target population has been vaccinated, and the frequency of genital warts among women has fallen between 70% and 90% depending on the region.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





