

Experimental drug developed by researchers at Stanford University and University of São Paulo protected rats against persistent damage to cells that leads to chronic heart failure (photo: Alda-1 reduced post-MI damage in experiments with rats / release)
Experimental drug developed by researchers at Stanford University and University of São Paulo protected rats against persistent damage to cells that leads to chronic heart failure.
Experimental drug developed by researchers at Stanford University and University of São Paulo protected rats against persistent damage to cells that leads to chronic heart failure.
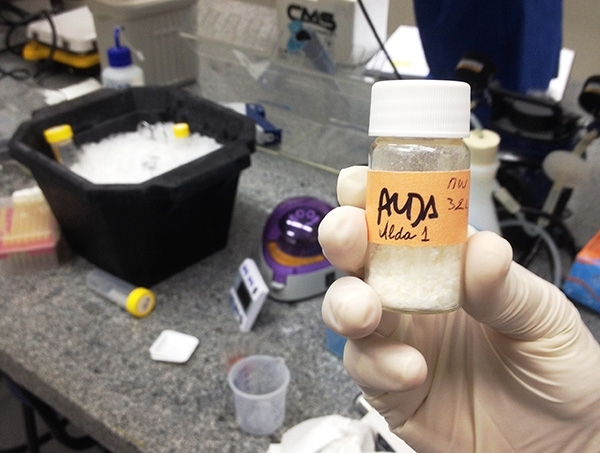
Experimental drug developed by researchers at Stanford University and University of São Paulo protected rats against persistent damage to cells that leads to chronic heart failure (photo: Alda-1 reduced post-MI damage in experiments with rats / release)
By Karina Toledo
Agência FAPESP – Following myocardial infarction, rats were treated with an experimental drug called Alda-1 that reduced heart function impairment by almost half in experiments performed at the University of São Paulo (USP). The results were published in the International Journal of Cardiology.
Alda-1, a synthetic molecule developed by the collaborative efforts of researchers at Stanford University in the United States and the University of São Paulo’s Biomedical Science Institute (ICB-USP) in Brazil, is capable of activating ALDH2 (aldehyde dehydrogenase-2), a mitochondrial enzyme essential to the proper functioning of all cells, including those of the heart.
The first clinical trials to test the safety of this compound are in progress in the US with funding from private support.
“The enzyme ALDH2 is essential for metabolizing aldehydes, which are highly reactive molecules that impair the production of cellular energy (ATP) when overproduced by the organism and cause a release of other reactive substances, such as free radicals and even more aldehydes,” said Julio Cesar Batista Ferreira, a professor in ICB-USP’s Anatomy Department and the coordinator of the research project, which is supported by FAPESP.
In a previous study in rats with heart failure, the group had shown that treatment with Alda-1 increased the heart’s blood-pumping capacity (read more at: http://agencia.fapesp.br/19463).
In the new study, which was also performed as part of Kátia Maria Sampaio Gomes’ research for her master’s degree, Alda-1 was administered on the day after infarction and was found to significantly reduce the persistent damage to cells that leads to chronic heart failure.
“Before treating the animals, however, we set out to understand what happens to the heart’s aldehyde metabolism after myocardial infarction. We wanted to see whether ALDH2 activity changes, whether this affects aldehyde accumulation and whether it really influences the progression of the disease,” Ferreira said.
In the animal model that was used in the study, acute myocardial infarction (MI) is simulated by ligation of a coronary artery. The resulting diminution of blood supply causes immediate death to approximately 30% of heart cells. The remaining cells must work twice as hard to compensate for the injury, and they ultimately collapse. In this model, the animals typically show signs of heart failure approximately one month after MI induction.
To assess the progression of the disease, the researchers measured cardiac function, the metabolic profile of the heart (ATP production), ALDH2 activity and aldehyde levels in the blood and heart tissue during the first, second and fourth weeks after MI.
“We observed that without therapeutic intervention heart function steadily fell during the four-week period. Before MI, the cardiac ejection fraction was 81%. At the end of the first week, it was 54%. After the fourth week, it fell to 44%,” Ferreira said.
Steady impairment of ATP production and reduced ALDH2 activity were observed in heart cells that remained viable after MI. Blood aldehyde levels, which averaged 1.5 nanomoles per liter (nmol/L) before MI, rose to 2.8 nmol/L after the first week and 5.0 nmol/L at the end of the fourth week post MI.
“We found an inverse correlation in the sense that heart function diminished as blood aldehyde rose,” Ferreira said. “This suggests that ALDH2 was not working properly even though its expression did not decrease.”
These findings were validated in humans. In tests performed at USP, patients who had suffered acute MI presented with higher blood aldehyde levels than healthy individuals.
Heart biopsies from patients with ischemic, Chagas or idiopathic cardiomyopathy showed a reduction in ALDH2 activity and an accumulation of aldehydes. Findings from these studies on humans have not yet been published.
According to Ferreira, these trials suggest that physicians can use blood aldehyde levels as a marker of heart failure to assist them in diagnosing the disease and evaluating its progression.
Protective treatment
In another group of rats, treatment with the experimental molecule Alda-1 started on the day after the MI induction procedure. Four weeks later, cardiac function had fallen from 75% to 62%. Blood and cardiac tissue aldehyde levels were equivalent to those of the control group and thus in line with the levels that are expected for a subject with a healthy heart.
“The drug could not avoid heart function impairment completely because a large number of cells died during infarction, and treatment began only on the following day. Nevertheless, at the end of the experiment, blood pumping capacity was twice as high in the treated group as in the untreated group, showing that the treatment was protective,” Ferreira said.
Alda-1 was discovered during Ferreira’s tenure as a post-doctoral fellow at Stanford University, which was supported by FAPESP.
Led by Daria Mochly-Rosen, a professor at the Department of Chemical & Systems Biology, the Stanford group established Aldea Pharmaceuticals as a startup with Alda-1 as its lead drug candidate for commercialization.
Phase I clinical trials began in the US in late 2014 with healthy volunteers, solely to evaluate toxicity.
Aldea is initially focused on using the compound to treat alcohol intoxication, especially in patients with Alcohol Metabolism Deficiency (ALMD), which is caused by a single gene mutation in ALDH2 that makes the enzyme less functional. As a consequence, large quantities of aldehyde are released during alcohol metabolism.
This is the most frequent gene mutation known to science, affecting some 600 million Asians and people of Asian descent worldwide and approximately 45% of East Asians. The researchers at ICB-USP and Stanford recently published a review of the literature in the Annual Review of Pharmacology and Toxicology (ARTP) in which they advocate personalized medical care for these patients.
“Carriers of this gene mutation are more susceptible not just to the harmful effects of alcohol but also to tobacco, pollution, food rich in saturated fats and certain drugs that favor aldehyde production. Therefore the mutation makes them likely to develop a number of degenerative diseases,” Ferreira said.
In the ARTP article, the group presented a questionnaire that enables physicians to determine whether a patient has the mutation without the need for genetic testing. The article also offers a list of drugs that patients carrying the mutation should avoid.
“We’ve known about this mutation for many years, but it’s never been considered a factor capable of influencing the progression of a disease. By developing a tool to activate ALDH2, we managed to show its importance to the organism,” Ferreira said.
Extended scope
Ferreira’s group is currently performing preclinical studies in partnership with Aldea Pharmaceuticals to extend the scope of ALDA-1’s applications to other degenerative conditions of ischemic origin, such as peripheral arterial disease.
“Working in synergy with startups is a highly rewarding experience that stimulates the process of transferring the knowledge and technology that is created in academia for the benefit of society,” Ferreira said.
The group is searching for Brazilian partners who are interested in clinical application of Alda-1. These studies are being conducted as a part of the Supernova Program, an initiative of ICB-USP researchers who partner with researchers at Stanford to professionalize and boost innovative academic projects.
The paper “Aldehydic load and aldehyde dehydrogenase 2 profile during the progression of post-myocardial infarction cardiomyopathy: Benefits of Alda-1” (doi: 10.1016/j.ijcard.2014.10.140) can be read at www.sciencedirect.com/science/article/pii/S0167527314020774.
The paper “A personalized medicine approach for Asian Americans with the Aldehyde Dehydrogenase 2*2 variant” (doi: 10.1146/annurev-pharmtox-010814-124915) can be read at www.annualreviews.org/doi/full/10.1146/annurev-pharmtox-010814-124915?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





