

Experiments in rats showed researchers that implants containing layered double hydroxides did not induce inflammation but instead accelerated the healing process. The arrows show where LDHs with magnesium (left) and zinc (right) were implanted (image: Scientific Reports)
Experiments showed researchers that implants containing layered double hydroxides did not induce inflammation but instead accelerated the healing process.
Experiments showed researchers that implants containing layered double hydroxides did not induce inflammation but instead accelerated the healing process.
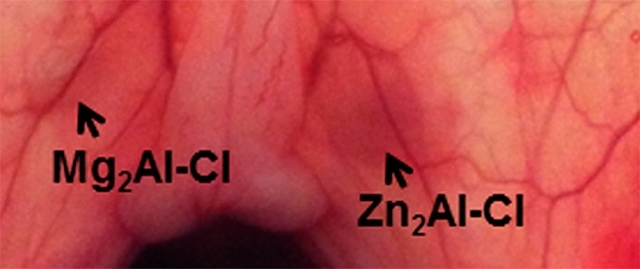
Experiments in rats showed researchers that implants containing layered double hydroxides did not induce inflammation but instead accelerated the healing process. The arrows show where LDHs with magnesium (left) and zinc (right) were implanted (image: Scientific Reports)
By Karina Toledo | Agência FAPESP – Layered double hydroxides (LDHs) are inorganic nanoparticles made up of layers of elements such as magnesium, iron and aluminum. Recent research suggests that these materials, also called anionic clays or hydrotalcite-like compounds, can be used for controlled drug delivery.
With FAPESP’s support, researchers at the University of São Paulo (USP) and the Federal University of São Paulo (UNIFESP) in Brazil performed experiments with rats to test the biocompatibility of implants containing LDHs. Analysis conducted during a 30-day period following the surgical procedure showed that the nanoparticles did not induce inflammation but instead accelerated tissue healing around the wound.
The results of the study, performed during Vanessa Roberta Rodrigues da Cunha’s postdoctoral research, were published in Scientific Reports.
“Most toxicity tests with this kind of inorganic material are done in cell cultures. We opted for in vivo testing because we were thinking of future applications in humans. For example, it would be interesting for local treatment of inflammation,” said Vera Regina Leopoldo Constantino, a professor at the University of São Paulo’s Chemistry Institute (IQ-USP) and the principal investigator for the study.
LDHs can be found in nature or synthesized in the lab with a high degree of purity using elements present in the human body, such as zinc, magnesium and iron as well as aluminum, Constantino explained. The layers of which the material is made are positively charged and must be neutralized by placing a negatively charged species, such as chloride or carbonate, between them.
“LDHs made of magnesium, aluminum and carbonate are marketed by pharmaceutical companies as antacids. The idea of replacing carbonate with a drug began to be explored in the scientific literature in 2001. The layers can be used to convey the drug into the human body,” Constantino said.
Several studies have shown that the layers protect the drug, she explained, potentially extending its shelf life and assuring the controlled release of the active principle inside the organism to avoid peaks that could cause side-effects.
“Some studies also show that because the layers slow down drug degradation in the organism, it should be possible with this carrier to use smaller doses of the active principle, which would also help reduce side-effects. First of all, however, we need to prove that the material is biocompatible and won’t trigger an inflammatory process in the organism,” she said.
Neovascularization
The experiments in animals were performed in collaboration with Ivan Hong Jun Koh at the São Paulo Medical School (EPM-UNIFESP). Professor Koh and his group have studied the circulatory dynamics of microvessels, which have a diameter of less than 100 nanometers.
Tablets with a diameter of 5 millimeters (mm) and a thickness of 2 mm that contained LDHs without drugs of any kind were implanted in the abdominal muscle of healthy young adult rats. This region was chosen because it is highly vascularized, and any inflammatory process that occurred could easily be detected.
One group of animals received a tablet made of magnesium, aluminum and chloride, while LDHs of zinc, aluminum and chloride were implanted in another. The healing process was monitored for 30 days and compared with the process in two other groups – a negative control subjected to the same surgical trauma but not given an implant and a positive control implanted with a polypropylene surgical mesh with recognized antigenicity (in other words, the capacity to produce an inflammatory response).
“We used a novel approach known as sidestream dark field or SDF videomicroscopy to evaluate the formation of new blood vessels around the implant,” Koh said. “This is important because when there is inflammation, new blood vessels aren’t formed, and the walls of the existing microvessels are affected, potentially resulting in the formation of thrombi with a reduction in local vascular density.”
SDF videomicroscopy can also be used to measure the number of blood vessels formed and detect their functional and structural characteristics, as well as the blood flow dynamics.
“The circulatory dynamics were just as good in both groups of rats that received the LDH implant as those in the negative control group,” Koh said. “We found that the zinc LDH stimulated neovascularization of the tissue more than the other LDH. In the positive control group, we observed vascular lesions.”
Histological analysis showed that whereas there was no tissue reconstruction due to inflammation in the positive control, the healing response after 30 days in both groups that received LDHs was even better than that in the negative control. According to Koh, this finding can be explained by the presence of zinc and magnesium, which are essential to cell metabolism and the structuring of proteins.
“The group that received the LDH with zinc displayed even more pronounced cell growth than the group implanted with the magnesium LDH, as well as a different, looser type of collagen. This is interesting as it shows the possibility of controlling the type of protein that will be formed around this carrier in accordance with need in each case,” Koh said.
The results point to the significant potential applicability of LDHs as drug carriers and even as stimulants of cell proliferation, he added.
Next steps
The first tests of LDH implant biocompatibility were performed in healthy muscle tissue. According to Constantino, new experiments are currently underway using tablets that contain a substance capable of causing inflammation in tissue as well as LDHs that contain an anti-inflammatory drug. The results of these studies will be published shortly.
The article “Accessing the biocompatibility of layered double hydroxide by intramuscular implantation: histological and microcirculation evaluation” can be read at nature.com/articles/srep30547.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





