

Methodology developed in Brazil combines low-intensity electric current with a formulation containing nanoencapsulated chemotherapy (image: fibroin film contaning peptide / release)
Methodology developed in Brazil combines low-intensity electric current with a formulation containing nanoencapsulated chemotherapy.
Methodology developed in Brazil combines low-intensity electric current with a formulation containing nanoencapsulated chemotherapy.
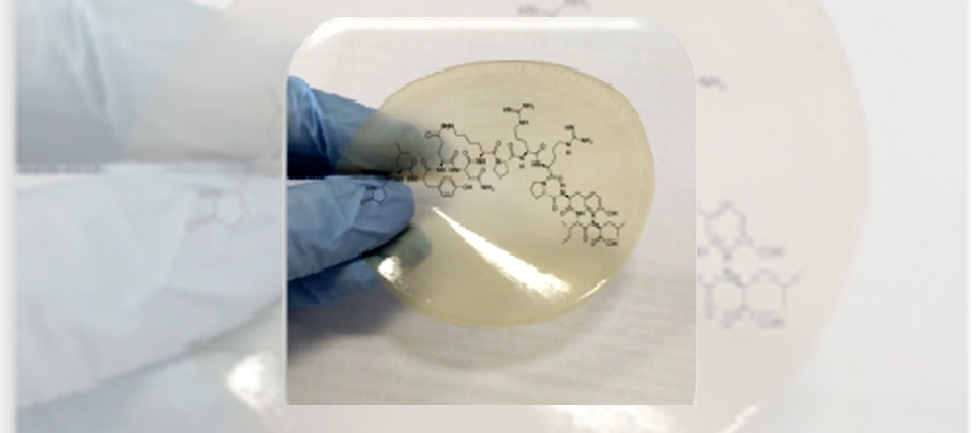
Methodology developed in Brazil combines low-intensity electric current with a formulation containing nanoencapsulated chemotherapy (image: fibroin film contaning peptide / release)
By Karina Toledo, in Lubbock (USA) | Agência FAPESP – Researchers at the University of São Paulo (USP), in Brazil, are testing a technique in mice that combines low-intensity electric current with a formulation containing nanoencapsulated chemotherapy to treat skin cancer.
Preliminary results of the study were presented in the United States during FAPESP Week Nebraska-Texas, held September 18-22, 2017, in the cities of Lincoln (Nebraska, USA) and Lubbock (Texas, EUA).
“One of the challenges involved in this type of topical treatment is ensuring that the drug penetrates the stratum corneum – the outermost layer of the epidermis, composed mainly of dead cells. It is an important tissue barrier against the entry of microorganisms, but it also makes it more difficult for medicines to penetrate,” explained Renata Fonseca Vianna Lopez, a professor at the School of Pharmaceutical Sciences of Ribeirão Preto (FCFRP-USP).
Applying a low-intensity unidirectional current is one of the ways to ensure that chemical substances penetrate the skin, pushed into the bloodstream through the electric field using a technique known as iontophoresis.
In the case of skin cancer, however, the intent is not that the drug penetrates the tissue to get into the bloodstream, but rather that it becomes concentrated in the area below the stratum corneum that requires treatment. This is the reason why, in the study led by Lopez, she chose to place the chemotherapeutic agent inside nanoparticles.
The study has been conducted under the scope of a Thematic Project funded by FAPESP. Initial in vivo tests were carried out during Raquel Petrilli doctorate.
Using mice, the researchers induced formation of a tumor associated with one of the most common types of skin cancer – squamous cell carcinoma – through a subcutaneous injection of human tumor cells that overexpress the epidermal growth factor receptor (EGFR). Lopez explained that the presence of this protein causes the tumor to become more aggressive.
The treatment was conducted using a formulation containing chemotherapy agent 5-fluorouracil encapsulated in a nanoparticle (liposome) that functions as an anti-EGFR antibody. The malignant cells are able to capture a larger quantity of the drug encapsulated in these liposomes.
One group of rodents received the tumor formulation through subcutaneous injections and another group received it through topical application combined with iontophoresis.
The group that received the formulation combined with iontophoresis presented significantly greater reduction in the size of the tumor than those that received it through injection.
“In addition to reducing the size of the tumor, the topical treatment left the tumor less aggressive. We believe that this method combined with iontophoresis allows the drug to be dispersed over the entire area of the tumor, whereas the subcutaneous application causes it to be concentrated in a single location,” Lopez noted.
Versatile technique
In another study, Lopez’ group used a stiffer type of polymeric nanoparticle, one containing the anti-inflammatory dexamethasone associated with iontophoresis for the treatment of uveitis – an inflammation of the eye tissue. The results, published in 2015 in the Journal of Controlled Release, is the outcome of the doctoral thesis of Joel Gonçalves Souza, winner of the 2015 Capes Thesis Award in Pharmacy.
“When we apply the medicine directly to the eye, it is quickly eliminated through the defense mechanisms, such as tears. Increased penetration and better results are obtained by using the application method combined with iontophoresis,” Lopez said.
Currently, in dissertation research by Camila Lemos, the group plans to test a method that uses iontophoresis in the treatment of chronic wounds such as those that develop in patients with diabetes.
“In this case, we are not dealing with the stratum corneum barrier. We use iontophoresis to assess its influence on release of the substance of interest in a formulation, and to investigate its effect on the growth of microorganisms,” Lopez explained.
The strategy consists of placing a peptide having anti-inflammatory properties on a film made of fibers extracted from the cocoon of a silkworm (fibroin). The film is placed on the wound as a dressing, to which an electric current is then applied.
“When we placed the peptide directly on the wound, it degraded very quickly. When placed on the film, however, release occurs in a slower and more sustained way. Iontophoresis allows a larger amount of the peptide to be released from the film at the start of treatment to accelerate healing,” the researcher explained.
Lopez went on to say that preliminary results suggest that iontophoresis also stops the proliferation of some types of microorganisms (particularly gram-positive bacteria) that could aggravate wounds.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





