
Brazilian experiments show that consumption of five times the recommended dosage of iodine is sufficient to reprogram gene expression in offspring
Brazilian experiments show that consumption of five times the recommended dosage of iodine is sufficient to reprogram gene expression in offspring.
Brazilian experiments show that consumption of five times the recommended dosage of iodine is sufficient to reprogram gene expression in offspring.
Brazilian experiments show that consumption of five times the recommended dosage of iodine is sufficient to reprogram gene expression in offspring
By Karina Toledo
Agência FAPESP – A Universidade de São Paulo (USP) experiment conducted in rats has shown that excessive consumption of iodine during pregnancy and lactation can make offspring more likely to suffer from hypothyroidism in their adult lives.
Funded by a FAPESP fellowship, the study is part of the post-doctoral research project undertaken by Caroline Serrano do Nascimento, who was supervised by Professor Maria Tereza Nunes of USP’s Biomedical Sciences Institute (ICB-USP).
“The deleterious effects of acute or chronic excess iodine in an organism are described in the literature. We are now evaluating whether this element also sets off epigenetic mechanisms. Excessive consumption of this element during gestation or lactation generates consequences for fetal development and apparently programs the offspring to be more susceptible to the development of hypothyroidism during adult life,” commented Nascimento.
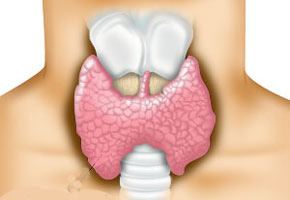
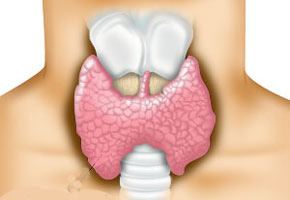
Iodine is an essential micronutrient for humans and all other mammals because it is used in the synthesis of the thyroid hormones T3 (triiodothyronine) and T4 (thyroxine). In addition to regulating metabolism, these hormones are important for the normal functioning of nearly all organs.
For decades, scientists have known that iodine deficiency can cause goiter – an increase in the thyroid gland’s volume that can limit its function. It is also well known that a lack of iodine during gestation can cause brain damage in children because thyroid hormones play an extremely important role in the development of the central nervous system. For this reason, Brazil made the addition of iodine to table salt mandatory in 1950.
However, recent studies have shown that consuming higher levels than the recommended daily dose of 150 micrograms could also cause a loss of thyroid function. This year, an ANVISA resolution reduced the range of iodine in salt from 20 to 60 milligrams per kilogram to 15 to 45 milligrams per kilogram, based on the recommendations of the World Health Organization (WHO) for populations that consume up to 10 grams of salt per day.
The measure was implemented following new research by the Health Ministry showing that the Brazilian population ingests greater levels of iodine than what is recommended by the WHO owing to higher salt consumption.
In her master’s and doctoral research, Nascimento studied what happens in organisms during acute iodine overload. “Scientists have known that acute excess has an inhibitory effect on the thyrocyte – a thyroid cell that produces thyroid hormones – since 1948. This rapid and adaptive effect serves to protect the cell against the momentary overload. The objective of my master’s and doctoral research was to uncover the molecular bases of this phenomenon,” she explained.
Nascimento showed that excess iodine reduces the expression and activity of a protein known as NIS, which is responsible for transporting this essential oligo-element for the biosynthesis of thyroid hormones by thyrocytes.
“When NIS [a sodium iodine symporter] gene expression is reduced or is not working appropriately, the thyrocyte captures less iodine and produces fewer hormones. However, after the period of inhibition or overload ends, the cell begins to synthesize and secrete hormones normally,” she said.
Data from the literature and another study conducted at the ICB under Nunes’ coordination, however, indicate that when excessive iodine consumption becomes chronic, the thyrocyte loses the capacity to adapt and escape the inhibitory effect.
“When we treat rats chronically with excess iodine, we observe a reduction in the expression of several proteins related to thyroid hormone synthesis and an increase in protein expression related to thyrocyte function. In addition, there is an increase in the production of inflammatory cytokines, which could set off thyroiditis,” explained the researchers.
According to Nascimento, there are studies that have reported an increase in the incidence of autoimmune thyroiditis, such as Hashimoto’s disease, in response to excess iodine in food.
Genetic reprogramming
Knowing the effects of chronic exposure to excess iodine and cognizant of the importance of thyroid hormones in pregnancy, Nascimento and Nunes decided to investigate the effects of an overload during this important period of development. They sought to evaluate whether the losses caused by excess iodine in a mother could be transmitted to her offspring via epigenetic mechanisms.
According to Nascimento, in the first trimester of gestation, the fetus is completely dependent on the thyroid hormones produced by the mother, and any alteration in hormonal synthesis in this phase could have serious consequences for fetal development. After the second trimester, the baby has its own developed thyroid but still depends on iodine from the mother, which is transferred through the placenta.
“As the placenta expresses the NIS protein, we wanted to discover whether excess iodine could hamper the transportation of this element to the fetus. Additionally, during lactation, this transportation could be compromised by an iodine overload because the breast also expresses NIS. Another of the study’s objectives is to investigate whether treating the mother with excess iodine could alter gene expression in offspring or hamper development,” explained Nascimento.
From the beginning of gestation to the end of lactation, rats received water containing five times the recommended dosage of iodine. In the case of humans, this dosage is equivalent to ingesting the iodine found in 12 grams of salt (before the ANVISA resolution). The control group received solely the quantity of iodine that is considered to be ideal.
“We opted for a dose equivalent to what could be consumed by the Brazilian population, which is known to consume a very large quantity of salt,” explained Nascimento.
After weaning at 21 days of life, the offspring in the two groups began to receive rations and water containing the ideal quantity of iodine. At 90 days of age, the researchers found that the rat offspring submitted to overloads of the mineral had developed hypothyroidism, whereas the offspring in the control group had healthy thyroids. The mothers treated with excess iodine presented symptoms of hypothyroidism, as was expected, at the end of the lactation period.
“We observed that the majority of the genes linked to the biosynthesis of thyroid hormones had reduced expression in both the mothers and their offspring in the group exposed to excess iodine during gestation and lactation,” explained Nascimento.
The next step, according to the researcher, is to discover at what moment in gestation or lactation this excess iodine is more prejudicial. “Once we have clarified the mechanisms that occur in offspring, we can discover in what phase of development iodine alters genetic programming in animals. Apparently, for each of the phases, there is a different response in the programming of gene expression during adult life,” she affirmed.
Despite knowing the consequences of excessive iodine ingestion, Nascimento does not recommend eliminating or reducing its addition to salt. “Ideally, there would be investment in public policy to reduce salt consumption in the population to avoid not only thyroid function losses but also cardiovascular disease. In contrast, with the current reduction, there is no guarantee that people will ingest ideal quantities of iodine,” she stated.
According to the researcher, a better understanding of the way that the NIS protein is regulated by iodine could offer interesting therapeutic prospects.
“NIS is extremely important in the diagnosis and treatment of thyroid cancer with radioactive iodine. Many studies have attempted to increase the expression of this protein in cancerous tissue so that the tissue can capture more radioactive iodine and the therapy will be effective. As such, understanding how this protein is regulated can offer interesting prospects in the development of therapies aimed at treating thyroid cancer or other types of cancer,” she affirmed.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





