

In experiments on rats performed at the University of São Paulo, the experimental drug called rostafuroxin improved artery relaxation capacity by 50% and reduced blood pressure levels (image: Blausen gallery 2014/Wikiversity Journal of Medicine)
In experiments on rats performed at the University of São Paulo, the experimental drug called rostafuroxin improved artery relaxation capacity by 50% and reduced blood pressure levels.
In experiments on rats performed at the University of São Paulo, the experimental drug called rostafuroxin improved artery relaxation capacity by 50% and reduced blood pressure levels.
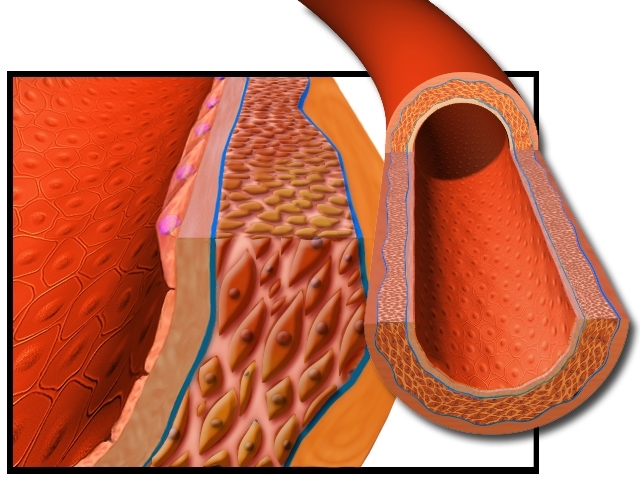
In experiments on rats performed at the University of São Paulo, the experimental drug called rostafuroxin improved artery relaxation capacity by 50% and reduced blood pressure levels (image: Blausen gallery 2014/Wikiversity Journal of Medicine)
Agência FAPESP – The treatment of hypertensive rats with the drug rostafuroxin – currently in clinical trials – has provided a 50% improvement in artery relaxation capacity, reversing oxidative stress observed in the endothelium and significantly reducing blood pressure rates in the animals.
The data, published in a recent article in the Journal of Hypertension, are from a FAPESP-funded study performed in the Department of Physiology and Biophysics at the Institute of Biomedical Sciences of the University of São Paulo (ICB-USP).
The line of research was presented by Professor Luciana Venturini Rossoni during the 29th Annual Meeting of the Brazilian Federation of Experimental Biology Societies (FESBE), held in Caxambu (MG) on August 27-30, 2014.
“Rostafuroxin is a drug that inhibits the action of ouabain, the hormone responsible for the fine control of sodium in the kidney, for volemia [the quantity of blood circulating in the body] and for the intracellular concentrations of calcium in the blood vessels and heart. Previous studies have shown that 45% of hypertensive patients present elevated concentrations of ouabain in the plasma,” Rossoni explained.
For nearly 20 years, the researcher has been devoted to the study of ouabain’s role in alterations of vascular reactivity (the capacity of the vessels to contract and relax) and in the development of high blood pressure.
Produced in specific areas of the central nervous system and in the suprarenal gland, ouabain is capable of inhibiting the action of the enzyme Na+/K+/ATPase – better known as the sodium-potassium pump – found in cell membranes and responsible for regulating the transport of these ions between intra- and extracellular media.
“The enzyme Na+/K+/ATPase is critically important for maintaining homeostasis [the physiological balance of the chemical composition of cellular fluids] in the cells. In the case of the blood vessels, it controls the intracellular concentrations of sodium and, as a result, maintains the optimal concentrations of calcium,” Rossoni explained.
In a 2011 article published in the Journal of Vascular Research, the ICB-USP group showed that it was possible to induce hypertension in healthy rats administered daily doses of ouabain for 20 weeks, until they achieved plasma concentrations similar to those observed in the plasma of hypertensive patients.
By investigating the effects of the treatment, the researchers observed that ouabain increased the contractibility of what are known as resistance arteries, or small vessels that control the passage of blood from the arteries to the capillaries and veins, thus hampering blood flow.
“We determined that by stimulating the activity of the cyclooxygenase-2 (COX2) enzyme, ouabain increased the production of vasoconstricting substances and reactive oxygen species. This increase in oxidants inside the cell in turn diminished the bioavailability of nitric oxide (NO), an important vasodilator agent released by the endothelium,” Rossoni explained.
In another study also published in the Journal of Hypertension, the scientists demonstrated that in rats genetically predisposed to developing hypertension – and with pressure levels already altered at the beginning of the study – daily treatment with ouabain was able to increase the reactivity of the arteries after just five weeks of treatment.
DOCA-salt model
In the more recent experiments, the goal of the ICB-USP group was to discover what would happen in the resistance arteries of hypertensive rats when treated with rostafuroxin. For this, the researchers used an animal model known as a DOCA-salt, in which they induced hypertension by increasing the circulating blood volume.
In this model, the rats undergo surgery to remove one of their kidneys and then receive weekly injections of the drug desoxycorticosterone, whose function is to increase the kidney’s reabsorption of sodium. In parallel, the rodents also begin to receive water with an increased sodium concentration.
“The blood pressure gradually increases until the fifth week and then stabilizes. After this period, the animals present severe hypertension, around 180 mm of mercury (mmHg),” Rossoni said.
As soon as the condition of hypertension was established, one subgroup of the animals began to receive daily oral doses of rostafuroxin, whereas the other subgroup received only a placebo. In just the first week of treatment, the group that received the drug presented a drop in blood pressure. After three weeks, the systolic pressure of the treated animals was between 140 and 150 mmHg, which could be considered mild hypertension.
“The tendency was for pressure to drop. It’s possible that the pressure would [even] return to normal levels if treatment were continued for a longer period,” Rossini speculated.
According to the researcher, the three-week administration of rostafuroxin had been agreed upon with Sigma-Tau Pharmaceuticals, the holder of the patent, so that the findings would be comparable with those of previous studies performed on the drug.
In investigating what had happened to the resistance arteries, which are of critical importance in controlling peripheral vascular resistance, the researchers observed a full reversal of oxidative stress and a 50% improvement in the relaxation capacity that was dependent on the function of the endothelial cells.
“In the hypertensive animals, the vessels did not relax as much as they should have. Treatment with rostafuroxin improved the condition but did not completely reverse it due to a higher release of nitric oxide in the endothelial cells and less degradation by reactive oxygen species,” Rossoni said.
Clinical trials
In previous clinical trials, scientists from the Sigma-Tau laboratory investigated the effects of rostafuroxin on kidney and heart tissue. The results showed that in the kidneys, the drug is capable of preventing the reabsorption of sodium induced by the administration of ouabain at concentrations similar to those found in the plasma of hypertensive patients. In the heart, however, the drug can prevent the formation of fibrosis and hypertrophy. The ICB-USP group was the first to investigate the vascular effects of the drug.
According to Rossoni, the Sigma-Tau laboratory has already conducted initial clinical trials with the medication, which were not successful because they included patients with cases of hypertension caused by other etiologies.
A second phase of clinical trials is including only patients whose hypertension is related to an increase in volemia, explained the ICB-USP researcher.
“We’re very hopeful in relation to the findings and believe that rostafuroxin will soon prove to be another option for treating cases of resistant hypertension, which generally require the use of a combination of three or more different drugs,” she said.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





