

A formulation could be used in patients at risk of respiratory failure to prevent their condition from deteriorating. This methodology has been used to treat HIV/AIDS by an international group of scientists led by Brazilian researchers (image: surface of a human dendritic cell / National Institutes of Health / Wikimedia Commons)
A formulation could be used in patients at risk of respiratory failure to prevent their condition from deteriorating. This methodology has been used to treat HIV/AIDS by an international group of scientists led by Brazilian researchers.
A formulation could be used in patients at risk of respiratory failure to prevent their condition from deteriorating. This methodology has been used to treat HIV/AIDS by an international group of scientists led by Brazilian researchers.
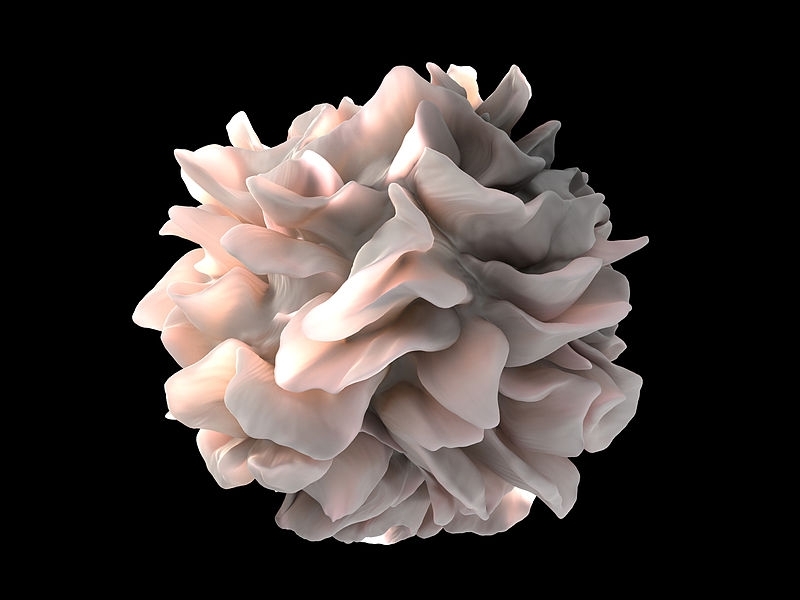
A formulation could be used in patients at risk of respiratory failure to prevent their condition from deteriorating. This methodology has been used to treat HIV/AIDS by an international group of scientists led by Brazilian researchers (image: surface of a human dendritic cell / National Institutes of Health / Wikimedia Commons)
By Karina Toledo | Agência FAPESP – A computational tool has helped Brazilian researchers affiliated with the Federal University of São Paulo (UNIFESP) and collaborators in other countries to develop a therapeutic vaccine against HIV, the virus that causes AIDS, that is currently being tested in patients in Brazil.
The group recently published an article on medRxiv in a unreviewed preprint version validating the computational platform and proposing adaptation of the methodology to create a formulation that can help patients recover from the severe form of COVID-19.
“The therapeutic vaccine would be indicated for patients who start displaying a fall in oxygen saturation, which can happen around seven days after the start of symptoms. The idea would be to prevent them progressing to respiratory failure,” said Ricardo Sobhie Diaz, a professor of infectious diseases at UNIFESP’s medical school (Escola Paulista de Medicina) and a coauthor of the study.
With support from FAPESP, Diaz has focused in the past eight years on looking for a “sterilizing cure” for AIDS, meaning the complete elimination of HIV from the body. Current treatment with a drug cocktail can reduce the viral load to zero, but the virus may rebound if the treatment stops.
One of the strategies researched at UNIFESP consists of training certain immune cells to “hunt” the virus in the host even if it is latent (inert inside lymphocytes and not replicating) or hiding in regions that cannot be reached by antiretroviral drugs. Italian, German and Egyptian scientists are participating in the project.
“We’ve developed a vaccine based on dendritic cells, also known as ‘antigen-presenting cells’. These defense cells teach T-CD4 lymphocytes to recognize particles of viruses, bacteria or any other invaders,” Diaz said. “CD4 cells in turn get CD8 lymphocytes, also called cytotoxic cells, to hunt down and eliminate cells infected by that specific antigen.”
In the UNIFESP study, dendritic cells are “trained” in the laboratory in a personalized manner for each patient. The researchers sequence the virus taken from the patient, focusing on the group-specific antigen (GAG), a region of the viral genome considered highly immunogenic.
Each patient’s genetic profile is also analyzed by sequencing the genes that encode human leukocyte antigens (HLAs). In this case, the aim is to discover which proteins are used by the dendritic cells to recognize and present the antigens.
“We developed a computational tool called Custommune, which analyzes the genetic data and selects epitopes [peptides made up of nine amino acids] capable of inducing a strong antiviral response in the individual concerned. We synthesize these peptides in the lab and have them interact in vitro with dendritic cells,” Diaz said.
The dendritic cells are obtained from a blood sample donated by the patient to be treated. The researchers process the blood serum to extract monocytes (a type of white blood cell), which they expose to certain cytokines (proteins that act as signals to the immune system) to induce the transformation.
The dendritic cells are then injected into each patient’s lymphatic system via the groin and underarms so that they can “train” the lymphocytes to eliminate the virus.
Promising results
The methodology was tested in ten patients who each received three doses of the vaccine. Preliminary analyses suggest that the formulation triggered an antiviral response in the host.
“After each dose, we collected another blood sample from the volunteers and extracted CD4 and CD8 lymphocytes,” Diaz explained. “These cells were put to interact in vitro with the viral peptides used to make the therapeutic vaccine. We observed that in this situation, lymphocytes began producing molecules such as interleukin-2, tumor necrosis factor alpha and interferon-gamma, all of which are proinflammatory cytokines characteristic of an antiviral response. With each dose of the vaccine, we observed a significant linear increase in cytokine production.”
As controls, the leukocytes from the patients were placed together with antigens from the bacterium Staphylococcus aureus, and in this case, no cytokines were produced.
All participants in the study had been taking an “AIDS cocktail” (antiretroviral therapy) for at least two years. It was not possible to evaluate the effect of the vaccine in terms of viral load suppression, as viral load was undetectable when the study began. Antiretroviral therapy was suspended during the study. In two participants, the virus was not detected in blood plasma in most of the samples collected for analysis.
The researchers now plan to conduct a clinical trial with 50 volunteers. Currently, this plan has been put on hold because of the pandemic. The proposal is to combine the therapeutic vaccine with the standard cocktail plus two drugs not normally used in AIDS treatment.
According to Diaz, in the case of COVID-19, the therapeutic vaccine would also have to be personalized for each patient. “For the article, Italian scientist Andrea Savarino [Università Cattolica del Sacro Cuore] simulated the use of the tool to select SARS-CoV-2 antigens that could be used in a formulation,” he said. “The computational platform can be used to develop vaccines based on dendritic cells, peptides or DNA.”
The article “Custommune: a web tool to design personalized and population-targeted vaccine epitopes” can be retrieved from www.medrxiv.org/content/10.1101/2020.04.25.20079426v1.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





