By Karina Toledo
Agência FAPESP – Cell therapy developed by researchers at the Universidade de São Paulo (USP) reduced liver regeneration time by half in rats subjected to surgery removing 70% of the organ.
The immediate goal is to test the effectiveness of the method in the treatment of induced cirrhosis in animals. In the future, scientists intend to evaluate whether the treatment may be used in humans.
The stem cells used in the study were obtained from liver buds of 12 ½-day-old rat embryos, explained Maria Angélica Miglino, professor in the USP School of Veterinary Medicine and Zootechny (FMVZ) and coordinator of the
FAPESP-funded study.
“In mammals, a structure known as the primitive gut develops at the very beginning of gestation, upon which the buds that originate all the organs of the abdominal cavity—the liver, pancreas, bladder and bowel—will grow,” said Miglino.
The hepatic stem cells have a natural tendency to transform themselves into hepatocytes, and because of this, they would theoretically be safer and more efficient for use in regenerative treatment of the liver in comparison with any other type of stem cell.
“These cells have the potential to form a liver. Our goals were to discover when they are formed and the best time to remove them from the embryo and to cultivate them and use them to treat induced cirrhosis in rats,” said Miglino .
During the master’s degree studies of Amanda Olivotti at FMVZ under the direction of Rose Eli Grassi Rici, the researchers identified the ideal moment during gestation to obtain the stem cells, cultivated them and performed morphological characterization and histological analysis.
“The cells proved to be most prolific and were in a pluripotent state halfway through the 12th day after fertilization. They showed no neoplastic transformation or genetic errors,” said Olivotti.
The next step, which was undertaken during Olivotti’s doctoral research, was to induce liver failure in the animals to test the regenerative strength of the therapy.
“In the first group of rodents, 70% of the liver was removed. This causes a metabolic deficit and leads to insufficiency, resembling cases in which the organ is lost due to trauma. It also simulates a condition in which children are born with atrophied livers,” said Durvanei Augusto Maria, researcher at the Instituto Butantan’s Biochemistry and Biophysics Laboratory and co-advisor of the project.
In a second animal model, cirrhosis was induced through the administration of drugs that cause fibrosis in liver cells, causing symptoms similar to those caused by the excessive consumption of alcohol or chronic inflammation caused by illnesses like hepatitis.
Methods of administration
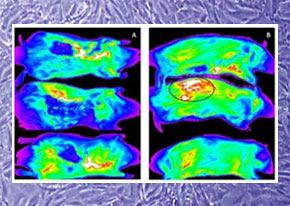
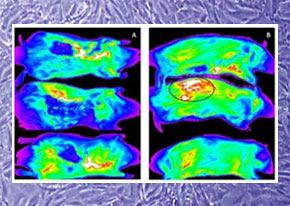
The researchers tested four different methods of administering the therapy to the hepadectomized rats. The stem cells were labeled with a fluorescent substance so that their path through the body could be monitored with ultrasound, x-ray and positron emission tomography (PET).
The first method evaluated was intravenous application, in which the cells were introduced into the organism through the penile vein. In a second group of rodents, the cells were injected into the peritoneum, the membrane that encases the organs in the abdominal cavity.
The third method tested was endotracheal, which consisted of inserting a catheter into the trachea and placing the cells into the lungs. “Some patients with cirrhosis develop a respiratory syndrome, and this would be an alternative for promoting improvement in the lungs first and then the liver,” explained Augusto Maria.
Last, the oral/enteral method was tested, in which a catheter was introduced through the oral cavity, the pharynx, esophagus and stomach, and the stem cells were then applied to the duodenum. According to Olivotti, the largest number of stem cells reached the liver by this method and remained in the organ for a longer period of time.
“We obtained the best results with the oral/enteral method because of the hepatic duct, the channel that connects the duodenum to the liver that is normally the passageway for bile. No one had tested this pathway until now,” said Miglino.
According to Augusto Maria, the intention is to evaluate a fifth pathway of administration, which is more direct but involves more risk: the hepatic artery. “From a surgical point of view, it is easier to insert a catheter than manipulate an artery. However, we intend to evaluate this pathway as well, as the idea is to develop a treatment model that can be reproduced in humans,” he said.
The animals were monitored for 21 days. After this period, the stem cells administered through all the administration pathways were viable, with varied efficacy in terms of liver regeneration.
“A liver takes an average of 25 days to regenerate following a hepadectomy in experimental models. With the application of a single dose of undifferentiated stem cells from the hepatic bud to animals subjected to hepadectomy, the average was reduced to 10 days, showing that it is a highly effective system,” said Olivotti.
Although the animals’ livers had returned to their normal size, their functionality has not been evaluated by the researchers. “These analyses will be performed at the end of the doctoral research, but the in vitro results indicate that the organ maintained its capacity for metabolization,” said Olivotti.
The pilot model for cirrhosis induced by medications had to be reevaluated because the drug used the first time--dimethylnitrosamine (DMN)—was too aggressive, and few animals survived the experiment.
“We established a new induction protocol with thiocetamide (TAA), which is less aggressive, but the process of developing cirrhosis takes longer,” said Olivotti.
The researchers are currently developing a new induction model by hepadectomy, in which 90% of the liver is surgically removed. “This protocol is more invasive, so we can monitor the liver regeneration process over a longer period of time,” he explained.
Clinical application
While the strategy has been shown to be promising, there are still many obstacles to be overcome before the therapy can be tested in humans. The first is to discover a viable way to extract the cells from the hepatic bulb.
“Even if the law allowed for it, we cannot use embryos left over from assisted reproduction treatment because the primitive intestine has still not formed during this phase of development,” said Miglino.
While it would be technically possible to use cells from fetuses that have undergone either spontaneous or induced abortion, many ethical and legal questions would be involved.
“One possibility would be to develop a bank of cells from primates adapted to form human livers. However, we still need to investigate whether transplant between different species would be viable,” said Miglino.
Augusto Maria says many long-term studies on animals will still be necessary to evaluate all the risks this therapy holds. “It is possible that the application of the cells could induce the formation of thrombi and create infarcted areas. It could also cause tumor formation or induce autoimmune illnesses,” he explained.
He added that long-term studies are also necessary to understand whether the stem cells stimulate the damaged tissue to regenerate itself or whether they themselves proliferate inside the organ.
“One possible strategy would be to induce cirrhosis in pigs to evaluate the effects of cellular therapy. Pig livers are the most similar to human livers,” said Augusto Maria.
The preliminary results are under evaluation for publication. The study is connected to the Thematic Project titled “
O enigma vitelino” [The Vitelline Enigma], which is also under Miglino’s supervision.