
A hybrid molecule offers the benefits of thalidomide and hydroxyurea without showing the toxic effects of the original drugs
A hybrid molecule offers the benefits of thalidomide and hydroxyurea without showing the toxic effects of the original drugs.
A hybrid molecule offers the benefits of thalidomide and hydroxyurea without showing the toxic effects of the original drugs.
A hybrid molecule offers the benefits of thalidomide and hydroxyurea without showing the toxic effects of the original drugs
By Karina Toledo
Agência FAPESP – A drug developed by researchers at Universidade Estadual Paulista (Unesp) to alleviate the symptoms of sick cell anemia combines the benefits of thalidomide and hydroxyurea chemotherapy—which is used for chronic treatment of the disease—without any of the toxic effects of the original drugs.
The molecule, patented under the name Lapdesf1, has shown excellent results in trials in mice conducted at the Universidade Estadual de Campinas (Unicamp). Scientists at the two institutions are now seeking a partnership with pharmaceutical companies to conduct the first tests in humans.
“The study represents an advance for treatment of sickle cell anemia, considered an extremely neglected disease, and will help to reduce several symptoms in patients, like pain and inflammation,” commented Unesp-Araraquara researcher Leandro dos Santos, who is currently working to perfect the molecule in a research project (“Optimization, synthesis and pharmacological evaluations of new candidate drugs for treatment of symptoms of sickle cell anemia”) funded by FAPESP.
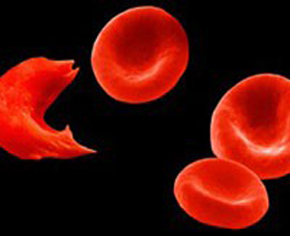
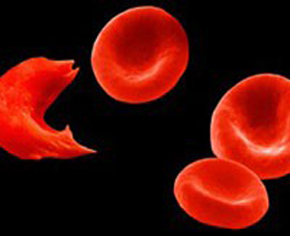
Sickle cell anemia is one of the most prevalent hereditary diseases in Brazil; it is estimated that more than 50,000 people are affected. Common in populations of African descent, it is caused by a genetic alteration in hemoglobin, a protein found in red blood cells that aids oxygen transport.
The mutation makes red blood cells take on the form of a sickle after oxygen is released to tissues. In low oxygen tensions, the cells become deformed and rigid, and they tend to aggregate, that is, form a cellular mass that sticks to the endothelium and makes blood circulation difficult, a process known as vascular occlusion.
In addition to chronic inflammation, the vascular occlusive process can cause necrosis in certain tissues and crises of intense pain. Ulcers on legs, dislocation of the retina, priapism (prolonged and painful erections), cerebral vascular accidents, heart attacks, kidney failure and lung failure are common effects of the disease. The disease also compromises bones and joints and tends to worsen with time, reducing life expectancy.
Hydroxyurea is one of the most widely used drugs in the treatment of sickle cell anemia because it increases production of another type of hemoglobin, fetal hemoglobin (present during uterine life). High levels of fetal hemoglobin reduce polymerization of defective blood cells and lower the risk of vascular occlusion.
Like any chemotherapeutic drug, however, hydroxyurea has side effects. In addition to causing nausea, abdominal pain, headaches, dizziness, sleepiness and convulsion, it can reduce production of bone marrow cells. It can also affect reproductive cells and lead to infertility.
Thalidomide, initially used as a sedative and antiemetic (a treatment for nausea), was withdrawn from the market worldwide in the 1960s after causing an epidemic of deformities in newborns. It was reintroduced in the 1990s to treat cancer, leprosy, lupus and AIDS. In Brazil, the use of thalidomide is restricted. The drug is produced by public laboratories and provided to patients under the National Health System (SUS).
According to Santos, in the case of sickle cell anemia, thalidomide is interesting owing to its anti-inflammatory effects. “We took advantage of the thalidomide subunit responsible for the beneficial anti-inflammatory effects and added a molecule responsible for the action mechanism of hydroxyurea, which is related to the capacity to donate nitrous oxide—the mediator responsible for the increase in fetal hemoglobin. In the tests of toxicity conducted thus far, Lapdesf1 has not shown any of the negative effects of the original drugs,” he said.
The initial design of the molecule was undertaken during Santos’s master’s studies, under the orientation of Professor Chung Man Chin, of Unesp-Araraquara’s School of Pharmaceutical Sciences. The results were published in 2011 in the Journal of Medicinal Chemistry.
During Santos’s doctorate work, funded in part through a FAPESP fellowship, the group perfected a molecule that modulates the speed of nitrous oxide donation. The data were released in 2012, again in the Journal of Medicinal Chemistry.
Pre-clinical trials
After preliminary experiments in vitro proved the therapeutic potential of Lapdesf1, the Unesp group formed a partnership with researchers at Unicamp’s Center of Hematology and Hemotherapy (Hemacentro) to conduct trials in mice that have been genetically modified to develop a condition similar to sickle cell.
The trials, conducted by researchers Carolina Lanaro and Carla Penteado, are being conducted under the auspices of a Thematic Project coordinated at Unicamp by Professor Fernando Ferreira Costa.
“The trials were conducted in a laboratory at Georgia Regents University in the United States because it was there that researchers had the most appropriate animal model for this type of test,” explained Penteado.
Approximately 20 rodents were split into two groups after reaching 3 months of age. Half were treated with Lapdesf1 for two months. The other half received only a placebo.
Penteado said, “In the treated group, the quantity of fetal hemoglobin doubled after this period—a similar result to that obtained with hydroxyurea. The quantity of inflammatory cytokines had fallen more than 70%—a similar effect to dexamethasone (a corticoid that is also used against inflammation). None of the animals had adverse side effects.”
While awaiting the possibility of initiating trials in humans, the Unicamp group has attempted to determine the exact activity of the new drug through new in vitro tests with animals. The results should be published soon.
New possibilities
Santos and Man Chin, for their part, continue working to perfect the molecule. In a FAPESP-funded study, the researchers selected three variants of synthesized drugs during their doctoral studies and added elements that can have another interesting effect in the treatment of sickle cell, namely, inhibiting platelet aggregation.
“We introduced a spacer between the two subunits of the molecule—thalidomide and hydroxyurea—that also had biological action,” Santos explained. “Metaphorically speaking, it would be like placing a spring to connect two balls. This spacer was used to improve recognition of the substances by bioreceptors.”
Preliminary tests conducted in vitro and in mice have shown that the new version of the drug has the same anti-inflammatory, analgesic and nitrous oxygen donation properties and is also capable of impeding platelet aggregation, which should also reduce the risk of vascular occlusion.
Santos also coordinates another research project, funded by FAPESP and the pharmaceutical company GlaxoSmithKline, the objective of which is to develop a drug with the same therapeutic potential as Lapdesf1 but does not have structural similarity to thalidomide. Unicamp and Unesp are participating in the ongoing project.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





