
The experiments focus on finding the most efficient immunization method for use in humans
The experiments focus on finding the most efficient immunization method for use in humans.
The experiments focus on finding the most efficient immunization method for use in humans.
The experiments focus on finding the most efficient immunization method for use in humans
By Karina Toledo
Agência FAPESP – A Brazilian vaccine against HIV, the virus that causes AIDS, will be tested in monkeys in the second half of this year. With trials slated to last 24 months, the experiments focus on finding the most efficient immunization method for use in humans. After the conclusion of the testing stage, if there is enough financing, the first clinical trials could begin.
Named HIVBr18, the immunizant was developed and patented by researchers, including Edecio Cunha Neto, Jorge Kalil and Simone Fonseca, from Universidade de São Paulo’s Medical School (FMUSP). Currently, the project is being conducted under the auspices of the Institute of Immunology Studies, one of the National Science and Technology Institutes (INCTs), a program of the Ministry of Science, Technology and Innovation (MCTI) that is funded by FAPESP in São Paulo State.
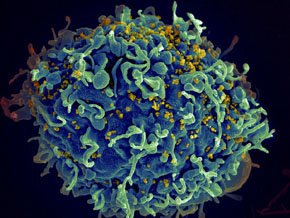
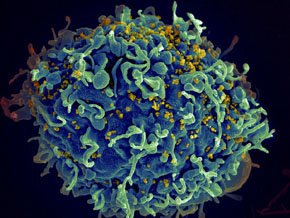
The study began in 2001 with funding from FAPESP’s Regular Grant program, under the coordination of Neto. In partnership with Kalil, the researcher analyzed the immune system of a special group of HIV+ individuals who have kept the virus under control for longer than average and have taken longer to get sick. The CD4 T cell count – which HIV targets when attacking the immune system – remains at a higher level than normal.
“We already knew that TCD4 are responsible for activating CD8 cells, which are producers of toxins that kill infected cells. The CD4 cells activate B cells, which produce antibodies. However, later studies showed that a specific type of CD4 cell could also have cytotoxic effects on infected cells. The HIV+ individuals who had cytotoxic CD4 cells managed to keep their viral load under control in the chronic phase of disease,” commented Cunha Neto.
The researchers also isolated small bits of proteins from the best-preserved areas of HIV, which are stable in nearly every strain. With the aid of a computer program, the scientists selected the peptides that had the greatest chance of being recognized by CD4 cells in the majority of patients. The 18 chosen peptides were recreated in laboratories and codified within a plasmid, or a circular DNA molecule.
In vitro tests on the blood samples of 32 HIV+ people with varied genetic and immunological profiles showed that in more than 90% of cases, at least one of the peptides was recognized by CD4 cells. In 40% of cases, more than five peptides were identified. The results were published in the journal AIDS in 2006.
In another experiment, published in PLOS One in partnership with Daniela Rosa, of Universidade Federal de São Paulo (Unifesp), and Susan Ribeiro, of FMUSP, the peptides were injected into mice that had been genetically modified to express molecules of the human immune system. In this experiment, 16 of the 18 peptides were recognized and activated both CD4 and CD8 cells.
“We performed the experiment with four groups of mice. Each group expressed a different type of human leukocyte antigen (HLA) molecule, which is directly involved in recognizing the virus,” explained Cunha Neto.
The researchers then developed a version of the vaccine with elements preserved from all subtypes of HIV from the main group, denominated Group M, which could induce immune responses against fragments of all subtypes tested to date. The study was conducted during the doctoral studies of Rafael Ribeiro.
“The results suggest that a single vaccine could, in theory, be used in several regions of world, where different subtypes of HIV are prevalent,” stated Cunha Neto.
In the most recent, still unpublished test conducted in mice, the researchers evaluated the capacity of this new vaccine to reduce the viral load. “HIV normally does not infect mice, so we used the vaccinia virus – which is in the family of the virus causing variola – and placed the HIV antigen inside,” explained Cunha Neto.
In the animals that had been inoculated with the vaccine, the quantity of modified virus found in the mice was 50 times lower than in the control group. The researchers are now conducting experiments to discover whether virus destruction in fact occurs because of the activation of cytotoxic CD4 cells.
“We will immunize a mouse and inject the modified virus. Afterward, we will separate the produced lymphocytes and inject only CD4 cells into a second animal. A third animal will receive only CD8 cells. The two animals that received lymphocytes specific for the modified virus will be infected – as well as a fourth animal that will receive only a placebo – so that we can see which mouse can best clear the virus,” explained Cunha Neto.
The scientists estimate that in the current stage of development, the vaccine will not completely eliminate the virus in an organism but could maintain a viral load so low that an infected person will not develop AIDS or transmit the virus.
According to Cunha Neto, HIVBr18 can also be used to strengthen the effect of other vaccines against AIDS, such as those vaccines developed by a group led by the immunologist Michel Nussenzweig, of Rockefeller University in New York, which are targeted against an HIV protein called gp140.
“In an experiment conducted by the researcher Daniela Rosa, we observed that pre-immunization with HIVBr18 improves the response to the vaccine against a recombinant protein from the HIV gp140 envelope, which is responsible for virus entry into cells. A vaccine capable of inducing the production of antibodies against this protein could block HIV infection,” said Cunha Neto.
Rhesus monkeys
The last stage of the preclinical trials will be conducted in a colony of rhesus monkeys from the Butantan Institute, in a partnership that involves the researchers Susan Ribeiro, Elizabeth Valentini and Vania Mattaraia. The advantages of conducting tests in primates are similarity with the human immune system and the fact that these animals are susceptible to SIV, the virus from which HIV originated.
“Our objective is to test several immunization methods. In addition to the DNA vaccine that was originally created, we will inject our peptides into other vaccine viruses, like the chimpanzee adenovirus, yellow fever virus or MVA, and select the best combination of vectors,” stated Cunha Neto.
Data show, for example, that a vaccine based on recombinant adenovirus containing the same 18 fragments of HIV induces a stronger immunological response in mice than the DNA vaccine.
According to Cunha Neto, the objective is to verify not only which formulation best activates cytotoxic CD4 cells but also which vaccine aids in the CD8 cell response and production of antibodies against the gp140 protein of the viral envelope.
Phase I clinical trials should include a healthy population with a low risk of contracting HIV, which will be followed closely for several years. In addition to evaluating the safety of the immunizant, the objective is to verify the magnitude of the immune response that the vaccine can trigger and for how long the antibodies remain in an organism.
If the HIVBr18 vaccine is successful in this first clinical stage, this formulation could spark commercial interest. The scientists hope to attract private investors because the estimated cost of the research prior to clinical trials is R$ 250 million. To date, including FAPESP and federal government funding, approximately R$ 1 million have been invested in the project.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





