

Circulating tumor microemboli expressing TGF-BRI. Gray circles are pores of the membrane used to filter blood cells (image: Ludmilla Chinen / A.C. Camargo Cancer Center)
Brazilian researchers find molecules in patients’ blood indicating which cases are likely to progress to metastasis or develop local relapse after treatment. Study also points to a novel therapeutic target.
Brazilian researchers find molecules in patients’ blood indicating which cases are likely to progress to metastasis or develop local relapse after treatment. Study also points to a novel therapeutic target.
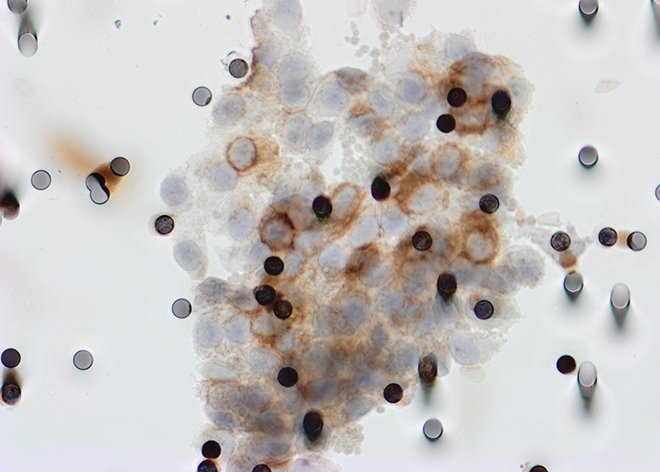
Circulating tumor microemboli expressing TGF-BRI. Gray circles are pores of the membrane used to filter blood cells (image: Ludmilla Chinen / A.C. Camargo Cancer Center)
By Karina Toledo | Agência FAPESP – Researchers at A.C. Camargo Cancer Center in Brazil have found markers in the blood of head and neck cancer patients that can help identify cases that are likely to evolve to metastasis or develop local relapse after treatment.
The results of the study, which was supported by FAPESP, were published in the journal Head & Neck.
“Besides pointing to new therapeutic targets, the findings can contribute to more personalized and effective treatment. If physicians know which patients run a heightened risk of progression of the disease, they can opt for systemic treatment with more powerful drugs,” said clinical oncologist Thiago Bueno de Oliveira, a co-author of the article.
Head and neck cancer is actually a group of tumors affecting the oral cavity (lips, tongue, floor of the mouth, and palate), paranasal sinuses, pharynx and larynx – in addition to glands, blood vessels, muscles and nerves in the region.
Head and neck cancer is most prevalent in developing countries, representing the ninth most common type of cancer in the world, with 700,00 new cases per year according to the International Agency for Research on Cancer, which is part of the World Health Organization (WHO).
In 2017, Brazil’s National Cancer Institute (INCA) estimated 22,000 new cases of oral cavity and laryngeal cancer, the most common types. Frequent use of tobacco and alcohol are the main risk factors, but in recent years, the number of cases associated with infection by human papillomavirus (HPV) has risen, especially among younger patients.
The group at A.C. Camargo decided to use liquid biopsy to understand how malignant cells separate from the primary tumor, enter the bloodstream and colonize other parts of the organism.
In liquid biopsy, body fluids, such as blood, saliva, urine and others, depending on the case, are analyzed for fragments of tumor DNA, small vesicles secreted by cancer cells, or circulating tumor cells (CTCs). The technique allows physicians to identify tumor characteristics and determine how the patient is responding to drugs at different disease and treatment stages.
The principal investigator of the study was Ludmilla Thomé Domingos Chinen, a researcher affiliated with A.C. Camargo Cancer Center’s International Research Institute (CIPE).
“In this specific case, we analyzed blood from 53 patients in search of CTCs, cells that escape from the primary tumor when it’s still developing and enter the bloodstream,” Chinen said.
All cases in the study were considered advanced based on tumor size or the fact that malignant cells had already begun to invade adjacent tissue, but the disease was still localized, i.e., not metastatic, and could be cured.
The researchers used a filtration device consisting of a membrane with eight-micrometer pores to separate CTCs from other blood cells. “The pores allowed through white and red blood cells and other normal blood cells, but most CTCs are 10-36 micrometers in diameter and were blocked by the membrane. We then looked at this material under a microscope,” Oliveira explained.
“Our group focused on analyzing these tumor cells in search of differentially expressed proteins that might be associated with resistance to treatment or the risk of metastasis,” Chinen said.
The first finding that drew the scientists’ attention was the fact that CTCs were present in more than 90% of patients with localized head and neck cancer. They were even more surprised to discover that the positivity rate remained stable in a second analysis performed after these patients had been treated with surgery, chemotherapy and/or radiotherapy (different combinations according to the type of tumor).
Furthermore, in 28% of cases, the CTCs were clustered in groups of three or more cancer cells known as circulating tumor microemboli (CTMs). As Chinen explained, CTMs can be considered organoids because in addition to CTCs they contain white blood cells, platelets, and other cell types. In the analysis performed after treatment the positivity rate for microemboli fell to 23%.
“We observed that the microemboli were always surrounded by platelets and began to suspect they were taking advantage of some factor released by these cells into the bloodstream. So, we decided to see whether the CTCs expressed a protein called TGF-βRI [transforming growth factor-β receptor I], a cytokine produced by platelets and involved in tumor growth,” Chinen said.
Therapeutic target
This stage of analysis found many CTCs in the isolate and showed that the CTCs that circulated as clusters of microemboli expressed TGF-βRI. “The patient positivity rate was 33% in the first analysis and 33% in the second. The proportion didn’t change after treatment, although the patients in question were different in each analysis. Some no longer expressed the protein and others had begun expressing it,” Oliveira said.
This rate and other factors, such as tumor size and progression, were then evaluated together using multivariate analysis while accounting for how long patients remained free from relapse after treatment.
The results showed that the presence of microemboli and cells expressing TGF-βRI in post-treatment analysis was correlated with a poor prognosis.
“The presence of TGF-βRI in the second analysis proved [to be] very bad for the patient. We had the impression that there was clonal selection in the sense that the cells that resisted treatment began expressing a molecule that enhanced the tumor’s capacity for invasion,” Chinen said.
The first (pretreatment) analysis showed that microemboli were present in 55% of the nine patients who progressed to metastasis. The group also found that patients with microemboli who received negative diagnoses after treatment remained free from relapse for at least 20 months.
Progression-free survival was 22.4 months in the most favorable cases, where both analyses were negative, and 17.5 months for patients who had negative results in the first analysis and positive results in the second. The worst cases were those involving patients with microemboli in both analyses, who remained free from relapse for only 4.7 months on average.
According to Chinen, one of the study’s most significant contributions is the indication that TGF-βRI is a therapeutic target in cases of head and neck cancer. “Outside Brazil, there are ongoing clinical trials with inhibitors of this receptor to treat other kinds of cancer,” she said.
“More research is needed to confirm our findings, but the study suggests that patients at heightened risk [positive expression of the receptor] could expect to prevent relapse if treated with this inhibitor,” Oliveira said.
He added that the study is being expanded as part of his PhD research and now includes 85 patients with the aim of obtaining more robust results.
The article, which is titled “Evaluation of incidence, significance, and prognostic role of circulating tumor microemboli and transforming growth factor-β receptor I in head and neck cancer” (doi: 10.1002/hed.24899), can be retrieved from ncbi.nlm.nih.gov/pubmed/28815787.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





