

Use of metformin correlates with reduced risk of head and neck cancer in study with more than 2,000 participants conducted at Brazilian university (1,1-dimethylbiguanide molecule / image: Wikimedia)
Use of metformin correlates with reduced risk of head and neck cancer in study with more than 2,000 participants conducted at Brazilian university.
Use of metformin correlates with reduced risk of head and neck cancer in study with more than 2,000 participants conducted at Brazilian university.
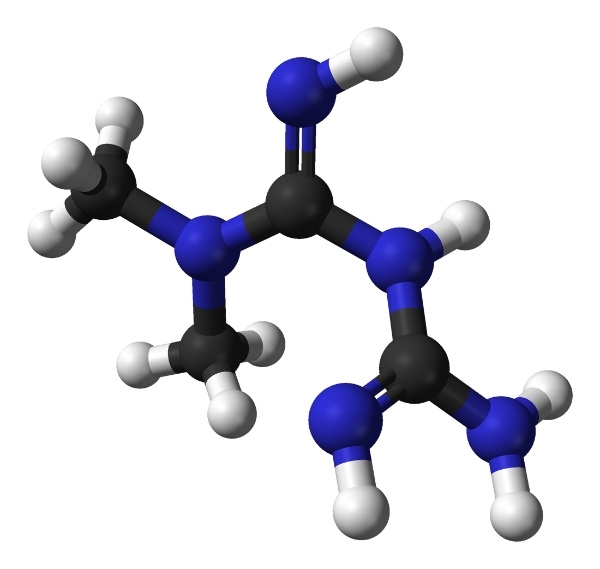
Use of metformin correlates with reduced risk of head and neck cancer in study with more than 2,000 participants conducted at Brazilian university (1,1-dimethylbiguanide molecule / image: Wikimedia)
By Karina Toledo | Agência FAPESP – In a study involving more than 2,000 volunteers in five hospitals in São Paulo State, Brazil, the use of metformin, one of the world’s most prescribed antidiabetic drugs, was found to be associated with a reduction in the risk of head and neck cancer.
The reduction was most pronounced – approximately 60% – among the volunteers considered at high risk for the disease because they consumed more than 40 grams of alcohol per day (equivalent to three cans of beer) and more than 40 packs of cigarettes per year.
The findings were presented by Victor Wünsch Filho, a professor at the University of São Paulo’s Public Health School (FSP-USP), at a conference on Next Frontiers to Cure Cancer organized by the A.C. Camargo Cancer Center, a Brazilian institution headquartered in São Paulo.
“Previous studies had already discovered an association between diabetes, use of metformin, and a reduction in the risk of other types of cancer, such as lung, colorectal and pancreatic cancer. In the case of head and neck tumors, however, the existing data in the scientific literature were highly contradictory, and we decided to investigate more thoroughly,” Wünsch said.
The case-control study was conducted during Rejane Figueiredo’s PhD research as part of Project Gencapo (the Portuguese-language acronym for Head and Neck Cancer Genome), which involves scientists affiliated with several Brazilian institutions and is supported by FAPESP.
The results were published in the journal Oral Oncology.
The study included 1,021 people with head and neck cancer, actually a heterogeneous group of tumors affecting the oral cavity (lips, tongue, floor of the mouth, palate), paranasal sinuses, pharynx and larynx, as well as glands, blood vessels, muscles and nerves in the region.
Head and neck cancer is most prevalent in developing countries and is the ninth most common type of cancer in the world, with 700,000 new cases per year, according to the World Health Organization (WHO). Smoking and alcohol are still considered the main risk factors, but in recent years, the number of cases associated with infection by human papillomavirus (HPV) has risen, especially among younger patients.
All cases of head and neck cancer in the study were placed in one of five subgroups: oral cavity, oropharynx, hypopharynx, larynx, and oral-oropharynx-hypopharynx unspecified.
The control group comprised 1,063 individuals without cancer who were visiting patients in the hospital or were admitted with conditions other than cancer, such as fractures or diseases related to the skin, eyes, or urinary tract.
“We excluded individuals with smoking- and alcohol-related diseases, as well as visitors to patients with head and neck cancer, because they were very likely to be exposed to the same risk factors as the patients themselves, and that could skew the results,” Wünsch said.
All participants answered a questionnaire on socioeconomic factors, demographics, lifestyle (including smoking and alcohol, among other items), and health (whether they had diabetes, used metformin, and had a family history of cancer, among other factors). Blood samples were also collected from cases and controls and used for glycated hemoglobin testing, one of the most accurate methods of diagnosing diabetes.
“We combined information from the questionnaires, medical records and blood tests for the purposes of statistical analysis. This is one of the unusual aspects of the study. If we had considered diabetes patients to be only patients with self-reported diabetes, the number would have been far smaller,” Wünsch said.
Participants with diabetes were divided into two subgroups depending on whether they used metformin. “We classed as metformin users only patients whose medical records contained this information. Therefore, volunteers who had come to the hospital as visitors were excluded even if they used metformin,” Wünsch said.
The analysis considering metformin use encompassed 1,021 cases (patients with head and neck cancer) and 587 hospital controls.
Diabetes and alcohol consumption
The statistical analysis showed that the proportions of smokers (68.0%) and drinkers (53.6%) were much larger among cancer cases than in the control group (16.3% and 43.5%, respectively). All told, 359 participants were confirmed as having diabetes: of these, 150 (14.7%) were cancer cases and 209 (19.7%) were controls.
Being diagnosed with diabetes was inversely associated with head and neck cancer in both men and women and in all subtypes of the disease considered in the study. However, risk reduction was statistically significant only for males (32% lower) and pharyngeal cancer (57% lower).
In general, the risk of having head and neck cancer was 46% lower for individuals with diabetes who used metformin than for participants without diabetes. No statistically significant risk reduction was found for individuals with diabetes who did not use metformin.
Among individuals who consumed relatively large amounts of tobacco and alcohol, those who had diabetes and used metformin were found to be 69% less likely to have cancer than nondiabetics.
“Initially, we thought of investigating just the association between head and neck cancer and diabetes. The idea of including metformin came up when I took part in a conference on cancer and metabolism, where I realized the drug’s importance. Put simply, it activates an enzyme called AMPK [AMP-activated protein kinase], which can inhibit cell proliferation,” Figueiredo said.
In her view, the findings point to the need for in-depth studies of metformin’s action on head and neck cancer.
“We need to understand more about the drug’s protection mechanism, usage time and dose by means of specific studies,” she said. “Only then will we be able to evaluate whether it can be used in cancer chemoprevention or to prolong the survival of cancer patients.”
According to Wünsch, so far, it has been possible only to assess the effect of metformin associated with diabetes, since diabetics are the drug’s main users.
“We already have evidence that the drug can have a significant protective effect in itself, and this needs to be studied in cancer prophylaxis as well as cancer treatment,” he said. “It’s an inexpensive drug with few side effects, so it could be interesting.”
The article “Diabetes mellitus, metformin and head and neck cancer” (doi: https://doi.org/10.1016/j.oraloncology.2016.08.006) by Rejane Augusta de Oliveira Figueiredo, Elisabete Weiderpass, Eloiza Helena Tajara, Peter Ström, André Lopes Carvalho, Marcos Brasilino de Carvalho, Jossi Ledo Kanda, Raquel Ajub Moyses and Victor Wünsch-Filho can be retrieved from sciencedirect.com/science/article/pii/S1368837516301348?via%3Dihub.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





