
Research at the University of São Paulo tests bone marrow stem cell transplants and are advancing the use of cellular therapy by taking different approaches for the treatment of insulin-dependent diabetes.
Research at the University of São Paulo tests bone marrow stem cell transplants and are advancing the use of cellular therapy by taking different approaches for the treatment of insulin-dependent diabetes.
Research at the University of São Paulo tests bone marrow stem cell transplants and are advancing the use of cellular therapy by taking different approaches for the treatment of insulin-dependent diabetes.
Research at the University of São Paulo tests bone marrow stem cell transplants and are advancing the use of cellular therapy by taking different approaches for the treatment of insulin-dependent diabetes.
By Karina Toledo
Agência FAPESP – Two studies underway at the University of São Paulo (USP) are advancing the use of cellular therapy by taking different approaches for the treatment of type 1 diabetes, also known as juvenile or insulin-dependent diabetes.
The most recent results of these studies were presented during the 7th Brazilian Stem Cell and Cellular Therapy Congress, sponsored by FAPESP and held in São Paulo at the beginning of October.
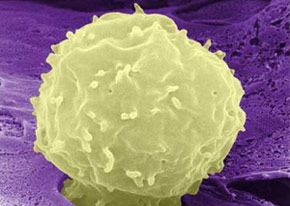
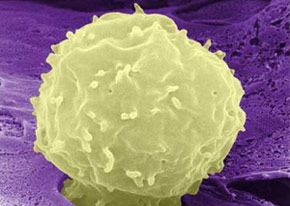
At the Cellular Therapy Center, part of the FAPESP Research, Innovation and Dissemination Center (CEPID) at the Ribeirão Preto Medical School (FMRP-USP), the strategy is to interrupt the destruction of the pancreas that occurs in type 1 diabetics through the use of hematopoietic stem cells extracted from the patient’s own bone marrow.
The immunologist Julio Voltarelli, who died in March 2012, optimized the technique. The study is continuing under the coordination of Maria Carolina de Oliveira Rodrigues and Belinda Pinto Simões. The endocrinologist Carlos Eduardo Couri is also contributing to the study.
“Type 1 diabetes is an auto-immune disease: the patient’s immune system attacks the cells that produce insulin in the pancreas. When the symptoms begin to appear, it is a sign that approximately 80% of the cells have been damaged,” explains Rodrigues.
If the destruction process is interrupted at this point and the remaining cells are preserved, according to researchers, the patient may be able to rid themselves of insulin dependence or at least reduce the necessary dosage.
“We are not talking about a cure, but about facilitating control of the disease and avoiding the complications of chronic diabetes, such as retinopathy, nephropathy and neuropathy,” comments Rodrigues.
With this objective, the first experimental protocol was initiated in 2004 with 25 patients. These patients underwent a procedure to collect and isolate hematopoietic stem cells from their bone marrow, and these cells were frozen. Then, the patients submitted to aggressive chemotherapy to destroy the remainder of the bone marrow and all blood cells (see article).
“The objective is to wipe out the immunological system to stop it from attacking the pancreas. Then, we infuse the frozen stem cells so that they can produce new bone marrow and new blood cells,” says Rodrigues.
According to the data presented by researchers during the congress, three of these 25 patients continue insulin-free. Another 18 had to begin taking the hormone again after a period of six months to five years, but they are receiving lower doses than before the treatment.
Another four patients did not manage to eliminate the need for insulin nor reduce their dosage. “Three of them had a history of ketoacidosis, a common complication in patients in the advanced stages of the disease. These volunteers probably did not respond to treatment because they no longer had insulin-producing cells to be salvaged,” explains Rodrigues.
Based on the preliminary data from the first experiment, the team began a new protocol in 2010. “The analysis indicates that chemotherapy was not strong enough to destroy all the blood cells in the patients, so we are testing a more aggressive treatment,” he comments.
To date, only two volunteers have received chemotherapy and the transplant. The team is currently accepting new applications (tmoautoimune@gmail.com) from candidates over the age of 18 who were diagnosed at least five months ago.
In another experimental protocol, initiated in 2008, the CTC researchers attempted to modulate the immunological system of eight diabetic patients through the application of mesenchymal cells.
“These cells are found in practically all organs of the human body and help support tissues, provide nutrients and produce growth factors,” comments Rodrigues.
In this case, the mesenchymal cells were extracted from the parent of the diabetic patient. Scientists hope that the cells will combat the inflammation of the pancreas and help regenerate the organ.
“There is also a third, less probable, hypothesis: that mesenchymal cells are capable of differentiating insulin-producing pancreas cells. Further study is needed,” he said.
The response, however, has not been encouraging in the first patients treated, and the team intends to begin a new experiment in 2013. “The idea is to apply greater quantities of mesenchymal cells. As this is a low toxicity treatment and does not involve chemotherapy, we can test it in patients aged 5 to 35,” says Rodrigues.
Protective capsule
At the Cellular and Molecular Therapy Center (Nucel), coordinated by Professor Mari Cleide Sogayar and affiliated with the Chemistry Institute and the Medical School of the Universidade de São Paulo, the strategy is to encapsulate pancreatic islets – sets of insulin-producing cells – with a biocompatible material that can prevent rejection after being applied to the the diabetic pancreas.
“The method has worked very well in tests with animal models. We implanted rat islets into mice to prove that the capsule is capable of preventing the destruction of the cells by the immunological system,” says Sogayar.
The capsule containing rat islets is implanted in the peritoneum, a membrane that coats the internal part of the abdominal cavity and covers organs such as the stomach and intestines. “We avoid the pancreas because it is very sensitive and easily inflamed. The islets begin to produce insulin in another region,” she explains.
After treatment, the diabetic mice were completely insulin-free, according to Sogayar. “After 250 days, we withdrew the capsules from the animals by washing the peritoneum and managed to show that the islets were intact. The mice then became diabetic again,” she said.
As a mouse lives for approximately one year, we can affirm that the treatment proved effective for almost the entirety of the rodent’s life. “But in humans, if necessary, the capsules can be substituted after some time,” says Sogayar.
To facilitate this procedure, the Nucel team is collaborating with the company CellProtect (a Nucel spin-off) in the development of a subcutaneous device that would store the capsules with islets and function as an artificial pancreas.
“The tube would be outside the skin and would facilitate the substitution of capsules when necessary. But we first need to discover how to maintain blood irrigation at the location. One possibility would be to use peptide factors such as recombinant human VEGF (vascular endothelial growth factor), which is already produced by Nucel,” explains Sogayar.
Although the idea of encapsulating islets has been developed in international studies, the team coordinated by Sogayar managed to perfect the method and create a biocompatible material containing a protein called laminin, which was patented under the name Bioprotect. FAPESP funded part of the study.
“The major advantage in terms of islet transplants, conducted with cells from a human donor cadaver for the type 1 diabetic patient, is that capsules dispense with the need for immunosuppressive drugs, which have significant side effects. Furthermore, there are few organ donors,” comments Sogayar.
“In the future,” she adds, “the idea is to transplant capsules containing different stem cells in insulin-producing cells or even pig islets in humans.”
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





