
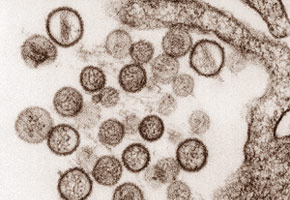
Aside from patenting the Araraquara hantavirus antigenic protein and distributing it throughout Brazil and South America, researchers from the University of São Paulo School of Medicine are investigating other emerging viruses including Oropouche and human Bocavirus (CDC)
Aside from patenting the Araraquara hantavirus antigenic protein and distributing it throughout Brazil and South America, researchers from the University of São Paulo School of Medicine are investigating other emerging viruses including Oropouche and human Bocavirus.
Aside from patenting the Araraquara hantavirus antigenic protein and distributing it throughout Brazil and South America, researchers from the University of São Paulo School of Medicine are investigating other emerging viruses including Oropouche and human Bocavirus.
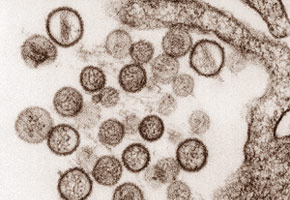
Aside from patenting the Araraquara hantavirus antigenic protein and distributing it throughout Brazil and South America, researchers from the University of São Paulo School of Medicine are investigating other emerging viruses including Oropouche and human Bocavirus (CDC)
By Frances Jones
Agência FAPESP – Doctors who have treated cases of hantavirus provide a striking description of the disease: within a matter of hours, a patient’s lung x-ray can progress from normal to that of a patient who is near death. What often begins as a simple fever progresses to serious pneumonia over a short time with little chance for reversal.
In 2012, the SUS National Health Plan registered 47 cases of the emerging disease, whose official name is Hantavirus Pulmonary and Cardiovascular Syndrome (SPCVH). It is transmitted by the inhalation of aerosols of the urine, saliva or feces of infected wild rats. Since its discovery in the Americas in 1993, some 1,600 cases have been reported in Brazil. These numbers are low in comparison to those of other illnesses, but the worrisome factor is its lethality: approximately half of those infected with the virus died.
Few medical centers in the country have the facilities necessary to study such a virulent microorganism. Among these few is the University of São Paulo Riberão Preto School of Medicine’s Center for Virology Research, which built a Biosafety Level 3 laboratory (the second-highest level on the scale) with FAPESP funding.
With funding from USP and FAPESP, the researchers submitted a patent request in 2006 (granted 2 years later) for an antigenic hantavirus protein produced at the center that stimulates the formation of specific antibodies when introduced into an organism. Today, the protein is used to diagnose the disease, but the goal is to create a vaccine based on this protein.
“Because it causes antibody production, its potential as a vaccine could be evaluated,” said researcher Luiz Tadeu Moraes Figueiredo, coordinator of a Thematic Project completed in 2012.
“We first need to know if the protein we produced protects animals from the infection. If it does, we will move forward until we can use it in humans. It’s a long process, but we’re going to get started,” he said.
A test based on the protein in question is the second method for hantavirus diagnosis to be developed at the center. The first method uses a relatively common technique: a real-time polymerase chain reaction that detects a sequence from the virus’ genome in a blood or tissue sample from the patient.
To produce the hantavirus protein, researchers selected a gene from the Araraquara virus - the strain that is most commonly responsible for hantaviruses in the Brazilian Cerrado (which extends from northeastern São Paulo State to southern Maranhão) - and transferred it to a bacterium.
The bacterium began to produce the protein, which was later purified by the scientists for use in diagnostic testing. The antibodies in patients’ blood are detected by an immunoenzymatic exam called ELISA.
“Both diagnostic methods are based on patient blood samples. In one, we look for the genome of the virus; in the other, we look for antibodies to the virus antigen that we produced in the laboratory,” said Figueiredo.
Other states and countries
Once patented, the recombinant Araraquara hantavirus protein was sent to other research centers in Brazil and abroad to help in the diagnosis and study of this type of virus.
Figueiredo describes studies based on the protein that have been carried out in Argentina and Colombia. “They are diagnosing hantavirus for the first time in Colombia, and they are using our protein to do it; they suspected that the illness existed, but they hadn’t diagnosed it. Now they’ve begun to do so.”
Pioneering cases are also being studied in the Brazilian states of Amazonas, Mato Grosso and Ceará. Scientists are seeking to understand which types of hantavirus circulate in these states; the illness can manifest itself in different ways and be transmitted by different types of rodents. According to Figueiredo, for example, the cases in Ceará do not seem to be as serious as those registered in São Paulo or Minas Gerais.
For now, Figueiredo says that the most lethal of the known hantaviruses is the Araraquara, whose vector is the rodent Necromys lasiurus, popularly known as the hairy-tailed bolo mouse, which is found in the Cerrado. “We found that this rodent loves the seeds of Braquiária grasses; they thrive in areas that are rich in these grasses.”
“We also showed that, in terms of the rodent, it seems that humans come into contact with the disease because of harm to the environment: when humans change the environment, certain species of rodents are selected, reducing diversity and allowing one species to predominate,” said Figueiredo.
Oropouche
Another virus that the scientists at the Centro de Pesquisa em Virologia de Ribeirão Preto are studying is Oropouche fever, which plays an important role in public health, especially in Amazonia.
“There have been over half a million cases of Oropouche infection in Brazil—second only in frequency to dengue fever arbovirus [which is transmitted by arthropod vectors such as mosquitoes],” said virologist Eurico de Arruda Neto, who is a main researcher on the Thematic Project, together with Benedito Antônio Lopes da Fonseca, Aparecida Yamamoto and Victor Hugo Aquino Quintana.
The virus causes an illness called Oropouche fever, which is similar to dengue fever. However, in approximately 5% of all cases, it can also cause meningoencephalitis.
Until recently, nobody knew how the virus killed the cells it infected. “We discovered in the studies carried out in the Thematic Project that the Oropouche virus actually kills the cell by inducing apoptosis, or programmed cell death. This apoptosis is mediated by the mitochondrial pathway and is dependent on a specific viral protein called NSs,” said Arruda.
Based on epidemiological and serological data, the researchers believe that the virus is changing its behavior and appearing in regions of Brazil outside of the North. “Doctors here in the Southeast aren’t familiar with this virus and don’t even study it in medical school because it’s an Amazonian virus. However, I think it’s much more common than we think in the Southeast. Because its outbreaks happen during the same season as dengue, doctors confuse the symptoms with dengue,” said Arruda.
To test the drugs and vaccines developed against Oropouche, the researchers created experimental infection models in hamsters and mice. “In both types of animal, the virus infected the central nervous system, affecting neurons and inducing their apoptosis. Aside from the central nervous system, the virus also replicates intensively in the liver, killing hepatic cells,” explained Arruda.
Over 4 years, some 60 people worked on more than 40 subprojects within the Thematic Project, which included studies on other recently discovered viruses such as the human bocavirus, which was first identified in Switzerland in 2005. In total, some 20 articles were published in international scientific journals, and the results were included in at least 8 doctoral theses and 15 master’s dissertations.
One of the high-impact articles within the Thematic Project, “A Global Perspective on Hantavirus Ecology, Epidemiology, and Disease” (doi: 10.1128/CMR.00062-09), published in Clinical Microbiology Reviews; it can be read at http://cmr.asm.org/content/23/2/412.full.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





