

Inflammation in the hypothalamus occurs a few days after excessive fat intake and is associated with the development of metabolic diseases (image: NIA/NIH)
In tests with rodents, researchers observed that the immune system attempts to mitigate damage to the hypothalamus caused by food, which can lead to obesity in the long term. Animals whose migration of these cells was inhibited experienced greater weight gain, increased fat accumulation, and worsened metabolic markers.
In tests with rodents, researchers observed that the immune system attempts to mitigate damage to the hypothalamus caused by food, which can lead to obesity in the long term. Animals whose migration of these cells was inhibited experienced greater weight gain, increased fat accumulation, and worsened metabolic markers.
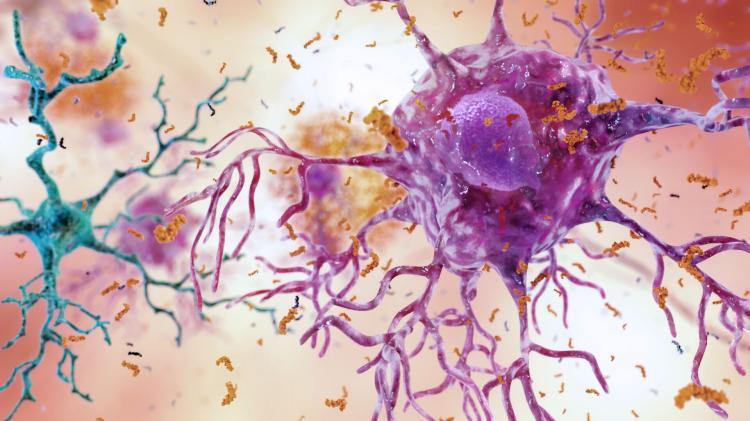
Inflammation in the hypothalamus occurs a few days after excessive fat intake and is associated with the development of metabolic diseases (image: NIA/NIH)
By Ricardo Muniz | Agência FAPESP – Several studies have shown that eating a high-fat diet induces an inflammatory response in the hypothalamus, one of the regions of the brain. This inflammation occurs a few days after excessive lipid intake and is associated with the development of metabolic diseases, such as obesity. At this time, a type of immune cell that resides in the brain called microglia plays an important role in the inflammatory response.
In a study published in the journal eLife, researchers from the State University of Campinas (UNICAMP) and their collaborators detailed how defense cells are attracted to the brain in the context of inflammation induced by a high-fat diet.
The research took place within the framework of the Obesity and Comorbidities Research Center (OCRC), a FAPESP Research, Innovation, and Dissemination Center (RIDC). It also received support from the Foundation through two other projects (17/22511-8 and 21/00443-6).
“In this work, we studied how the brain responds to a diet rich in fats, typical of modern Western diets, in which the consumption of fast-food and ultra-processed foods is quite frequent,” says Natália Ferreira Mendes, a researcher at the Department of Translational Medicine at UNICAMP’s School of Medical Sciences (FCM).
The study revealed that microglia are not the only defense cells involved in the process. Other immune cells that express a receptor called CXCR3 are also recruited to the brain when a high-fat diet is consumed. These cells come from outside the brain. This “reinforcement” appears to play a beneficial role by helping the microglia attenuate the inflammatory process and prevent obesity.
“We discovered this potential anti-inflammatory role of these cells through an experiment in which we blocked recruitment,” explains Mendes. “Immune cells are attracted to substances secreted in distant parts of the body, where inflammation occurs, and quickly head there. In simple terms, it’s as if someone sprayed perfume in a distant room of your house and you were directed there by the smell. What we did was prevent this ‘smell’ from being perceived and, as a result, many cells were unable to reach the inflamed site.”
The study found that animals whose defense cells were unable to reach the hypothalamus gained more weight, accumulated more fat, and exhibited worsening metabolic and biochemical markers. The group also identified differences in the recruited immune cells between males and females, which may influence how individuals of different sexes react to diet quality and how the immune system contributes to weight gain and related disease development.
Thus, the study helped to better understand the role of defense cells and the importance of the CXCR3 receptor in signaling them to reach the hypothalamus during inflammation, as well as their impact on metabolism in the context of diet-induced inflammation.
The diet used in the study is high in saturated fat, which is found in foods of animal origin, such as red meat and dairy products, as well as some foods of plant origin, such as coconut oil. Its solid or pasty consistency at room temperature makes it an attractive choice for the food industry, which uses it to improve the texture, consistency, and palatability of products.
“Consumption of this diet increases the concentration of free fatty acids in the blood, one of the ways in which fat is transported through the body. These fatty acids reach the hypothalamus, an area of the brain that’s particularly vulnerable,” says Mendes.
Unlike other brain regions, the hypothalamus comes into contact with an area called the median eminence, which lacks a blood-brain barrier. This barrier acts as a “wall,” protecting the brain from harmful substances in the blood. The blood vessels in the median eminence have “fenestrae,” or large pores, which allow various molecules, such as free fatty acids, to enter and quickly reach the hypothalamus. Additionally, the hypothalamus is located around the third ventricle, through which cerebrospinal fluid circulates. This makes it even more vulnerable to fluctuations in the concentrations of substances in this fluid. Therefore, the hypothalamus quickly detects excessive fat intake and activates the microglia in an attempt to control the damage caused by fatty acids.
However, when high fat intake is maintained over time, the microglia are unable to control the situation on their own. This is when immune cells summoned from other parts of the body step in.
Developments
Based on the results obtained, several questions arise for future research. One of the study’s approaches was comprehensive mapping of the genetic material of the microglia and cells recruited to the brain. “This type of analysis generates a valuable database that researchers around the world can access to investigate target genes involved in different physiological and pathological conditions,” says the researcher.
“With this, we provide the basis for many research projects to be developed, not only to better understand the role of microglia and other immune cells recruited in the context of obesity and inflammation in the hypothalamus, but also to explore the differences observed between females and males. Studying the origin of these differences in genetic material – considering aspects such as metabolic programming, hormonal changes, the effect of nutrients in the diet, among others – is a field that still needs to be explored in more detail.”
Mendes points out that, although the group’s findings are pioneering in showing how peripheral immune cells expressing the CXCR3 receptor are attracted to the brain in the context of inflammation induced by a high-fat diet, many questions remain. “For example, how do these recruited cells communicate with resident cells, such as microglia and neurons, among others? What are the long-term effects of recruiting these cells in the brain? What is the fate of these cells after the inflammatory process subsides? Are there peripheral hormonal or neural stimuli that help direct them to the brain? These questions need to be explored so that we can fully understand the mechanisms involved and develop more effective therapeutic approaches,” he says.
In any case, the discovery of a specific pathway for recruiting these cells to the brain opens up the possibility of developing drugs to treat obesity and associated comorbidities, such as type 2 diabetes.
In addition to Mendes, the paper is signed by Licio Augusto Velloso and Eliana Pereira de Araújo, who are from the OCRC’s Cell Signaling Laboratory (LabSinCel) and are the study supervisors. The other authors are Ariane Zanesco, Dayana C. da Silva, and Jonathan F. Campos (LabSinCel); Cristhiane Aguiar and Pedro de Moraes-Vieira (Immunometabolism Laboratory of UNICAMPs Institute of Biology); Gabriela Rodrigues-Luiz (Federal University of Santa Catarina); and Niels Olsen Saraiva Câmara (University of São Paulo).
The article “CXCR3-expressing myeloid cells recruited to the hypothalamus protect against diet-induced body mass gain and metabolic dysfunction” can be read at: elifesciences.org/articles/95044.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





