

The PRC2 inhibitor removes the “brakes” that prevent T lymphocytes from attacking cancer (image: Blausen Medical 2014/WikiJournal of Medicine)
A group led by researchers at the A.C.Camargo Cancer Center has succeeded in improving CAR-T cells, making them more effective in treating refractory types of lymphoma and leukemia.
A group led by researchers at the A.C.Camargo Cancer Center has succeeded in improving CAR-T cells, making them more effective in treating refractory types of lymphoma and leukemia.
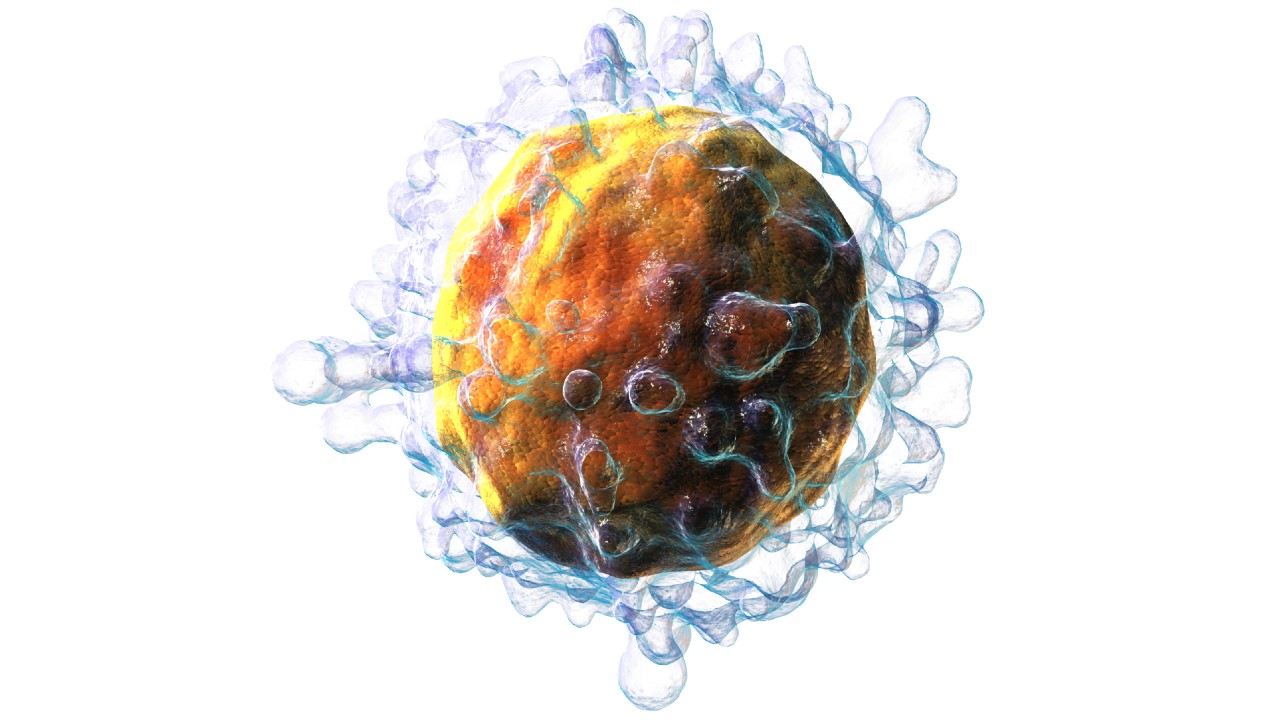
The PRC2 inhibitor removes the “brakes” that prevent T lymphocytes from attacking cancer (image: Blausen Medical 2014/WikiJournal of Medicine)
By André Julião | Agência FAPESP – Currently, half of patients with non-Hodgkin’s lymphoma and acute lymphoblastic leukemia – two types of cancer that affect blood cells – do not respond adequately to treatment with CAR-T cells. The therapy involves harvesting the patient’s own defense cells (T lymphocytes), modifying them in the laboratory to make them capable of destroying tumor cells, and reinjecting them into the body. These refractory cases usually relapse after conventional immunotherapy (read more at: agencia.fapesp.br/31675).
To overcome this problem, Brazilian researchers have developed a more powerful version of CAR-T cells. The details of the research were published in the journal Cancer Research.
“CAR-T cell immunotherapy is revolutionary and has saved many people’s lives in recent years. However, there are still a significant proportion of patients who don’t respond to this treatment. We tested a series of drugs on CAR-T cells and one of them showed promise by inhibiting the epigenetic alterations [related to the pattern of gene expression] that made the cells inefficient against these two types of hematological tumor,” says Maria Letícia Rodrigues Carvalho, first author of the study carried out at the A.C.Camargo Cancer Center with the support of a FAPESP Master’s Scholarship, now carrying out her doctoral studies.
As the authors explain, non-Hodgkin’s lymphoma mostly affects middle-aged adults, while lymphoblastic leukemia patients are mostly children.
The studies were conducted on tumor cells (in vitro) and mice (in vivo) and represent the first step toward future human trials.
Among the drugs tested on CAR-T cells, the one that showed the most potential was an inhibitor of the protein complex known as PRC2. In a healthy body, these proteins are necessary to induce the expression of genes that stop the action of defense cells so that they do not attack healthy cells.
“However, in the context of cancer, it’s important that there are no such brakes to completely eliminate the tumor. Although the basis of CAR-T cell immunotherapy is precisely to remove these brakes, some remain. What we did was to remove those that prevent a better response against non-Hodgkin’s lymphoma and acute lymphoblastic leukemia,” explains Tiago da Silva Medina, researcher at the A.C.Camargo Cancer Center, supported by FAPESP, and coordinator of the study.
Production
First, the researchers produced CAR-T cells from peripheral blood mononuclear cells of healthy individuals obtained from the blood banks of the A.C.Camargo Cancer Center in São Paulo and the National Cancer Institute (INCA) in Rio de Janeiro.
They also collected CAR-T cells produced from the blood of patients with the two tumor types and used in their own treatment at the A.C.Camargo Cancer Center.
The CAR-T cells were modified with the PRC2 complex inhibitor and used to treat (in vitro) the two types of tumor cells refractory to immunotherapy. As a result, the tumors were eliminated more quickly and efficiently than in samples treated with conventional CAR-Ts (without PRC2 inhibition).
The researchers then began testing mice that had developed both types of tumor. After treatment with the PRC2 inhibitor, the CAR-T cells were washed before being injected into the animals to ensure that there were no traces of the inhibitor, thus preventing the compound from targeting unwanted cells and reducing the risk of potential systemic toxicity. After 39 days, the animals that received the modified CAR-T cells had improved more than those treated with conventional cells.
“The modification made to the CAR-T cells induced a more persistent response in the organism and resulted in greater tumor elimination, both in vitro and in vivo. The epigenetic approach improves the quality of this immunotherapy and opens up a very promising perspective,” says Medina.
The researchers now plan to test the potential side effects of the therapy in mice. Approved treatments are known to exacerbate inflammation in patients. The problem is mitigated with drugs that are part of the immunotherapy protocol.
“If the new studies show that the treatment is safe, PRC2 inhibition could be incorporated into the production of CAR-T cells in the future, increasing the efficacy of the immunotherapy without increasing systemic risks,” concludes Carvalho.
The work was also supported by FAPESP through doctoral and post-doctoral grants awarded to some of the co-authors (22/00747-8, 20/10299-7 and 19/25129-2).
The article “Targeting PRC2 Enhances the Cytotoxic Capacity of Anti-CD19 CAR-T Cells against Hematological Malignancies” can be read at: aacrjournals.org/cancerres/article-abstract/doi/10.1158/0008-5472.CAN-24-1643/751986/Targeting-PRC2-Enhances-the-Cytotoxic-Capacity-of.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





