

Brazilian researchers discover one of the mechanisms of chemotherapy drug resistance in glioma and melanoma tumor cells and show that a combination of two drugs can make treatment more effective (image: glioma / Wikimedia Commons)
Brazilian researchers discover one of the mechanisms of chemotherapy drug resistance in glioma and melanoma tumor cells and show that a combination of two drugs can make treatment more effective.
Brazilian researchers discover one of the mechanisms of chemotherapy drug resistance in glioma and melanoma tumor cells and show that a combination of two drugs can make treatment more effective.
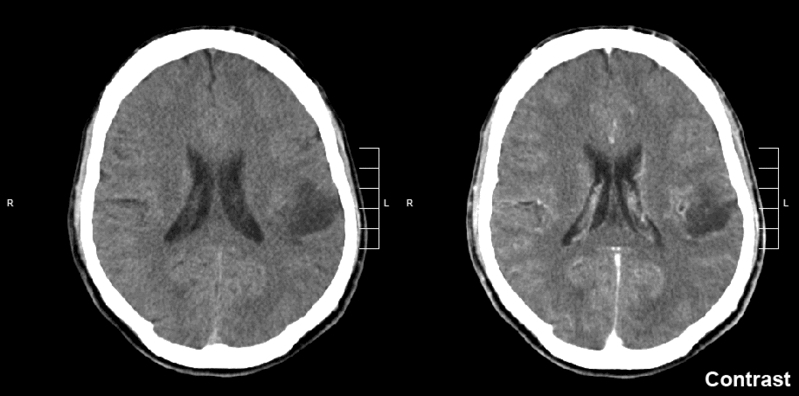
Brazilian researchers discover one of the mechanisms of chemotherapy drug resistance in glioma and melanoma tumor cells and show that a combination of two drugs can make treatment more effective (image: glioma / Wikimedia Commons)
By Elton Alisson | Agência FAPESP – Chemotherapy has limited success for patients with glioma – the most common kind of brain cancer – and melanoma – the most aggressive form of skin cancer – owing mainly to the resistance of tumor cells to the drugs currently available for such treatment.
Although this resistance is generally associated with the mechanisms by which tumor cells repair the damage to their DNA caused by chemotherapy drugs, according to specialists in the field, many other molecular factors are involved.
A group of Brazilian researchers from the University of São Paulo’s Biomedical Science Institute (ICB-USP) and the Federal University of Rio de Janeiro’s Carlos Chagas Filho Biophysics Institute (IBCCF-UFRJ) discovered during a study performed with FAPESP’s support that one of these factors is oxidative stress, caused by an accumulation of reactive oxygen species in the cells of tumors such as glioma and melanoma.
The researchers also showed that a combination of two drugs can enhance the effectiveness of the treatment to combat these two kinds of cancer.
An article on the study was published in the journal Oncotarget, and the study won the 8th Octavio Frias de Oliveira Prize in the Cancer Research category. The award was delivered in August 2017.
“The aim of the study was to understand why certain tumor cells are resistant to chemotherapy while others aren’t,” said Clarissa Ribeiro Reily Rocha, a postdoctoral fellow at ICB-USP with a scholarship from FAPESP and lead author of the article together with Carlos Frederico Martins Menck, a professor at ICB-USP.
With that in mind, the researchers analyzed four different glioma cell lines either sensitive or resistant to temozolomide (TMZ), a chemotherapy drug used as a first-line treatment for glioma and also used to combat melanoma by inducing DNA damage and potentiating levels of oxidative stress in tumor cells.
The analysis showed that the most drug-resistant cells displayed higher levels of glutathione, a peptide that plays a critical role in maintaining cellular redox balance by eliminating free radicals and that protects cells by inactivating their toxins.
“The problem, however, is that glutathione can also bind to drugs that attack tumor cells, inhibiting their action and expelling them,” Rocha told Agência FAPESP.
The researchers then set out to discover the reason for the higher levels of glutathione in TMZ-resistant cells. They found that these cells also expressed more of the protein NRF-2 (nuclear factor erythroid 2-related factor 2), a transcription factor that plays a crucial role in cells’ response against oxidative agents.
Other findings were that TMZ induces expression of NRF-2 in glioma cells and that NRF-2 in turn stimulates the production of glutathione to protect tumor cells from attack by the drug.
“We observed that NRF-2 plays a crucial role in resistance to TMZ via the synthesis and use of glutathione,” Rocha said.
Based on this discovery, they performed in vitro experiments with TMZ-resistant glioma cells and in vivo experiments in mice with injected tumor cells, silencing NRF-2 in order to find out whether this reduced resistance to the drug.
The results of these experiments showed that silencing NRF-2 increased the death of TMZ-resistant tumor cells.
“The idea now is to see if NRF-2 can serve as a molecular marker that indicates whether tumors in patients with higher expression of the protein are more likely to be resistant to chemotherapy, and also whether NRF-2 can modulate DNA damage repair in tumor cells attacked by these drugs,” Rocha explained. She recently completed a project designed to begin answering these questions at the Massachusetts Institute of Technology (MIT) in the United States with a scholarship from FAPESP for a research internship abroad (BEPE).
Experimental drug
The researchers also performed an experiment in which glioma and melanoma cell lines were treated with TMZ combined with buthionine sulfoximine (BSO), a glutathione synthesis inhibitor.
The results showed that this drug combination substantially increased the rate of death in TMZ-resistant cells.
“We found that the effect of the two drugs combined was synergistic – greater than the sum of their individual effects,” Rocha said.
To investigate whether the synergistic effect of TMZ combined with BSO also occurred in vivo, they inoculated the drugs both separately and together into different groups of mice with glioma and melanoma.
Nine days after the inoculation, they observed that tumor size had increased by a factor of 70 in the mice treated only with BSO and by a factor of 40 in the group treated only with TMZ.
In the group treated with the combination of the two drugs, progression of the cancer was significantly reduced, with tumor size increasing only tenfold over the entire treatment period.
“We’re proposing the use of BSO combined with TMZ to enhance the effectiveness of chemotherapy in treating glioma and melanoma,” Rocha said.
Clinical trials are currently under way to test BSO in combination with other chemotherapy drugs for the treatment of other kinds of cancer.
BSO has been approved in Phase II clinical trials, which assessed the drug’s efficacy and continued Phase I safety assessments in a larger group of patients.
“We plan to perform clinical tests with TMZ in combination with both BSO and other glutathione modulators. The priority is to modulate glutathione,” Rocha said.
The article “NRF2 and glutathione are key resistance mediators to temozolomide in glioma and melanoma cells” (doi: 10.18632/oncotarget.10129) by Rocha et al. can be read in Oncotarget at impactjournals.com/oncotarget/index.php?journal=oncotarget&page=article&op=view&path[]=10129&path[]=31876.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





