
Study carried out by USP researchers shows that patients with depression that present psychotic manifestations have altered cerebral structures and negative bias in memory for emotional information (FMRP-USP)
People suffering from depression oftentimes also present psychotic manifestations. But until now, the medical community had no objective methods to differentiate between these cases and cases of common depression, making the administration of specific treatment difficult.
People suffering from depression oftentimes also present psychotic manifestations. But until now, the medical community had no objective methods to differentiate between these cases and cases of common depression, making the administration of specific treatment difficult.
Study carried out by USP researchers shows that patients with depression that present psychotic manifestations have altered cerebral structures and negative bias in memory for emotional information (FMRP-USP)
By Fábio de Castro, do Rio de Janeiro
Agência FAPESP – People suffering from depression oftentimes also present psychotic manifestations. But until now, the medical community had no objective methods to differentiate between these cases and cases of common depression, making the administration of specific treatment difficult.
Correlating neuroimaging data and clinical tests, a group of researchers from the Universidade de São Paulo’s Riberão Preto School of Medicine (FMRP-USP) is taking the first steps toward defining the clinical and biological differences between psychotic and non-psychotic depression.
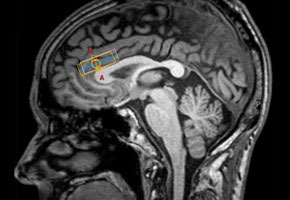
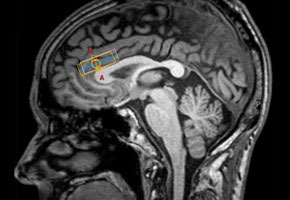
Preliminary data from a study coordinated by Cristina Marta Del Ben from the FMRP-USP Department of Neuroscience and Behavior show that patients with psychotic depression show changes in the volume of certain brain structures.
The study, which is part of the Thematic Project entitled “Typical and atypical neurotransmitters in neuropsychiatric disorders,” funded by FAPESP and coordinated by FMRP-USP’s Francisco Silveira Guimarães, was presented during the 26th Annual Meeting of the Federation of Experimental Biology Societies (FeSBE) in Rio de Janeiro on Friday August 26.
The study evaluated 23 patients with psychotic depression, 25 with non-psychotic depression and 29 healthy control subjects. The goal was to observe the differences between depression with and without psychosis. “But we thought it was important to correlate the results of biological alterations with clinical measures and finer psychic functions. That’s why we combined the data with a detailed clinical evaluation,” Del Ben told Agência FAPESP.
The neuroimaging data were obtained with a 3-Tesla scanner. The patients also underwent spectroscopy in order to detect the presence of a series of metabolites. The data were then analyzed by specific software.
“But we couldn’t limit ourselves to biological data, since it was necessary to consider the emotion and behavior involved in the manifestations of the disease. That’s why we also developed paradigms to evaluate the interferences in verbal and visual memory processing involving emotional stimuli,” said Del Ben.
In one of the tests, the patients had to memorize a list of 15 words with positive, negative or neutral meanings. A second list with 15 words was then presented and the participants had to identify which words were present on the first list. Another similar test was administered with positive, negative and neutral images. And a third test involved the identification of human faces expressing different types of emotions.
“Even though all the patients suffered from the same degree of depression, those that presented psychotic manifestations showed a greater tendency to pay attention to the negative. They didn’t notice positive stimuli that they had already seen, or they thought that they had seen negative stimuli that they actually hadn’t seen. It is as if they showed a bias for bad things,” said Del Ben.
Some brain structures in patients with psychotic depression showed changes in volume. The main difference happened in the isthmus of cingulate gyrus, which was reduced in these patients. According to Del Ben, this structure is part of the limbic system, a part of the brain responsible for emotions.
“The reduction in the posterior section of the cingulate gyrus was significant in the patients with psychotic depression, distinguishing them quite a bit from the non-psychotic patients. Plus, there is a correlation with the seriousness. The more serious the psychotic patient’s case, the smaller the structure was,” she pointed out.
Specific treatment
According to the scientist, the data are preliminary and were obtained about two months ago. “We just began making the correlations. But now we have data to make the connection between the changes in brain structure and this tendency to overestimate the negative side of things,” she affirmed.
The isthmus of the cingulate makes the connection between the occipital lobe—an important structure in visual processing and the perception of external stimulus—and the limbic system. According to the researcher, the study opens the way for looking at until what point depression with psychosis could be connected to a distorted perception of external stimulus.
“It’s one possibility that we are looking at. The possibility of a distorted perception of external stimulus is, in principle, coherent with the presence of delirium and hallucinations, which are typical of psychotic manifestations. We still need to explore the possibility of the problem with integration between the external world and subjective perception,” she explained.
According to Del Ben, it is possible that psychotic and non-psychotic depression are distinct conditions of mental disturbance that deserve specific approaches. That’s why it is important to study the difference.
“Understanding the physiopathogenics of the illness is fundamental for psychiatry. We are behind other medical specialties in that area. We need to deepen our understanding of the whole process to be able to intervene in the most appropriate manner. Today, patients are medicated with antidepressants that cause very unspecific changes in the whole brain. We still don’t know if it’s possible to use a more specific, personalized treatment,” she affirmed.
Aside from Del Ben, other participants in the study included post-doctoral researcher Maristela Schaufelberger Spanghero, currently teaching at FMRP, and Master’s students Aline Gerbasi Balestra and Helena Pinho de Sá.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





