
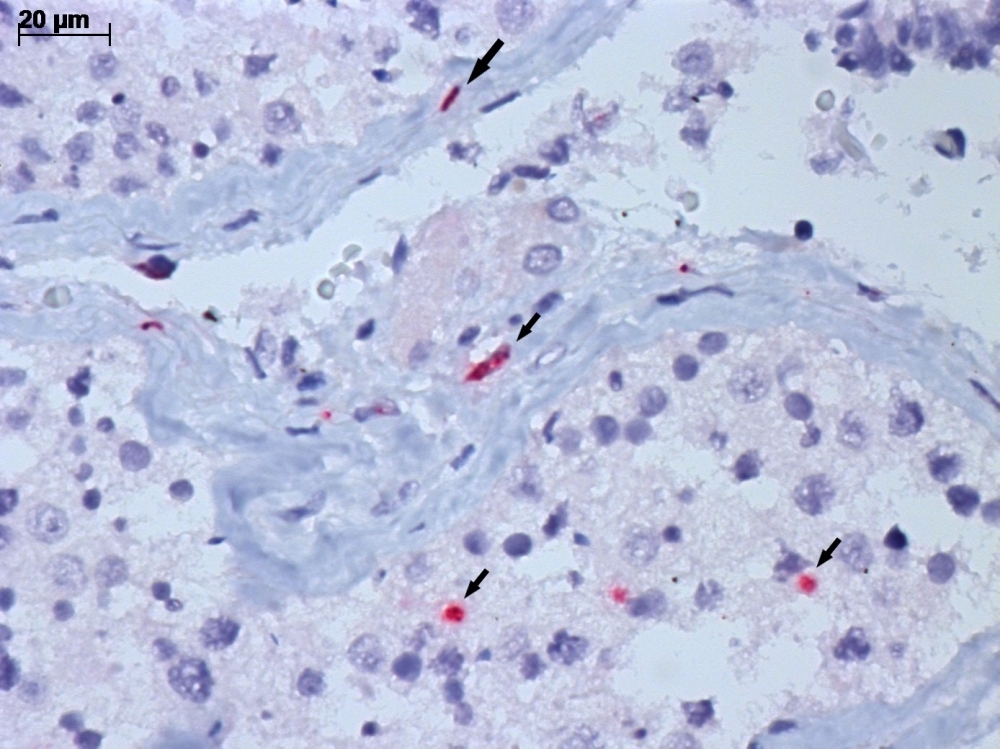
Microscope image of testicular tissue from deceased COVID-19 patient, obtained by minimally invasive autopsy. The image shows infection of several cell types by SARS-CoV-2. Arrows indicate the viral antigen (stained red) in infected cell cytoplasm (credit: Cristina Kanamura and Amaro N. Duarte-Neto/FMUSP and IAL)
Researchers at the University of São Paulo have found that infection by the novel coronavirus can cause lasting alterations to semen and testosterone production even in people who have mild or asymptomatic COVID-19.
Researchers at the University of São Paulo have found that infection by the novel coronavirus can cause lasting alterations to semen and testosterone production even in people who have mild or asymptomatic COVID-19.
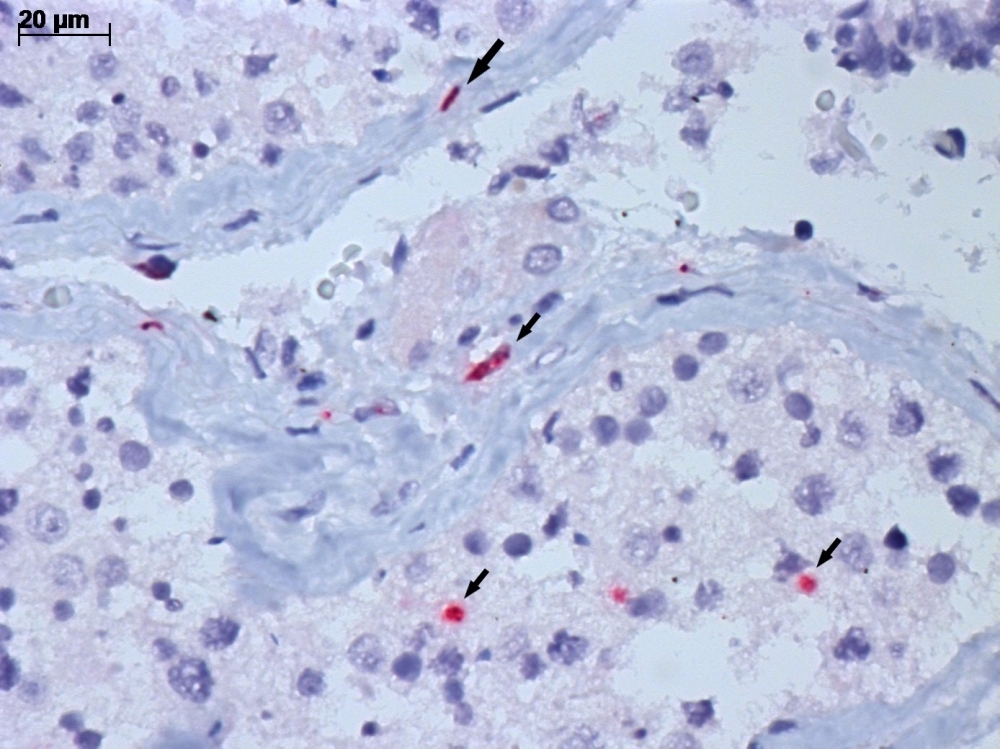
Microscope image of testicular tissue from deceased COVID-19 patient, obtained by minimally invasive autopsy. The image shows infection of several cell types by SARS-CoV-2. Arrows indicate the viral antigen (stained red) in infected cell cytoplasm (credit: Cristina Kanamura and Amaro N. Duarte-Neto/FMUSP and IAL)
By Elton Alisson | Agência FAPESP – While following up on male patients as they recovered from COVID-19 since the start of last year, andrologist Jorge Hallak, a professor at the University of São Paulo’s Medical School (FM-USP) in Brazil, noticed that their fertility and hormone tests continued to display alterations for many months after they recovered from the disease.
Several patients’ semen analysis results, for example, showed that sperm motility fell to 8%-12% (compared with more than 50% for healthy men) and remained at this level for almost a year after they were infected by SARS-CoV-2. Hormone tests showed testosterone levels also sharply down after the disease in many patients. Normal testosterone levels are 300-500 nanograms per deciliter of blood (ng/dL). In these patients, they were below 200 ng/dL, and in some cases as low as 70-80 ng/dL.
“We’re increasingly seeing long-lasting alterations in semen and hormone quality in COVID-19 patients, even when they had mild or no symptoms of the disease,” Hallak told Agência FAPESP.
Studies conducted in recent months by Hallak, in collaboration with colleagues in FM-USP’s Department of Pathology, have helped elucidate these observations made in clinical practice.
The researchers found that SARS-CoV-2 infects the testicles, impairing their production of sperm and testosterone. “It’s a cause of concern that the virus affects the testicles even in asymptomatic patients or patients with mild symptoms of the disease. Of all the agents that harm the testicles I’ve studied to date, SARS-CoV-2 appears to be the most active,” Hallak said. “Every pathology has peculiarities that experience and practice reveal to us. SARS-CoV-2 affects spermatogenesis [sperm production] in ways we’re discovering now, such as persistently low progressive motility without significant alterations to sperm concentration.”
Good sperm motility is critical to fertilization because it assures passage through the female reproductive tract and into the egg. Abnormally motile sperm cannot fertilize.
Ultrasound scans of 26 COVID-19 patients showed half to have severe inflammation of the epididymis, a long, coiled tube that transports sperm from each testicle. Sperm acquires its fertilizing ability and forward motility properties during epididymal transit.
The patients, whose age averaged 33, were admitted to Hospital das Clínicas, a hospital complex run by FM-USP, and tested by Instituto Androscience. The study was supported by FAPESP. An article reporting the results is published in the journal Andrology.
“In contrast with classic bacterial infections or other viral infections such as mumps, which causes testicular swelling and pain in a third of those infected, the epididymitis caused by SARS-CoV-2 is painless and can’t be diagnosed by visual inspection or palpation,” Hallak said, adding that testicular self-examination should be recommended as a public health policy in response to the pandemic.
“Ideally, adolescents, young adults and men at a reproductive age or who want to have children should consult a urologist or andrologist after being infected by SARS-CoV-2 to have all the relevant tests – measurement of testicular volume, testosterone and other hormones, semen analysis, and a sperm function test – followed by a color Doppler ultrasound scan to see if they have any kind of testicular abnormality that could affect fertility and hormone production,” Hallak said. “They should be followed up for at least one or two years after infection by the virus. We don’t yet know enough about these complications of the disease.”
Invasion of testicular cells
Another study recently published by the same group of researchers and also supported by FAPESP showed that SARS-CoV-2 invades all types of testicular cell, causing lesions that can impair hormone function and fertility.
Under the auspices of a project led by Paulo Saldiva and Marisa Dolhnikoff, both also professors at FM-USP, the researchers used a minimally invasive autopsy technique to extract testicular tissue samples from 11 men aged 32-88 who died at Hospital das Clínicas as a result of severe COVID-19. Analysis of the samples showed a number of testicular lesions possibly due to inflammatory alterations that reduce spermatogenesis and hormone production.
“What immediately drew our attention in these patients who died from COVID-19 was the drastic reduction in spermatogenesis. Even the younger ones at a reproductive age had practically no sperm,” said Amaro Nunes Duarte Neto, who heads the study. Duarte Neto is an infectious disease specialist and pathologist at FM-USP and Adolfo Lutz Institute.
According to Duarte Neto, the probable causes of reduced spermatogenesis in these patients include lesions caused by the virus in the vessels of the testicular parenchyma, with the presence of blood clots leading to hypoxia (low oxygen in the tissue), and fibrosis obstructing the seminiferous tubules, the part of the testicle in which sperm is produced.
A probable reason for reduced hormone production is loss of Leydig cells, interstitial cells that are located next to the seminiferous tubules and produce testosterone.
“The functions performed by the testicles, producing sperm and the main male sex hormone, are independent but connected because fertility declines if hormone production by Leydig cells is impaired,” Duarte Neto said.
Some symptoms of testosterone deficiency (hypogonadism), including loss of muscle mass, fatigue, irritability, memory loss and weight gain, can be confused with the long-term effects of COVID-19.
“An important part of this clinical condition is undoubtedly due to low testicular function, but the connection had never been made before because these patients don’t complain of pain and it isn’t routine practice to measure hormone production or analyze sperm after recovery from COVID-19,” Hallak said.
The researchers plan to conduct a follow-up study of male patients who have had the disease in order to find out if testicular lesions can heal naturally or be cured with medication. “We don’t know whether the lesions can be reversed or how long it would take,” he said.
His main concerns relate to men of reproductive age, adolescents and prepubertal children, given the lack of data on the testicular lesions caused by COVID-19. Nothing is known about the effects of the disease on puberty in terms of fertile capacity, whether hormone production is affected temporarily, for a long time or definitively, and the degree of irreversible residual damage.
Because there is no data on the condition of these male COVID-19 patients before they were infected, prospective studies should include a control group for comparison, Hallak suggested. “These subjects may have infertility problems and hormone alterations in future, and be unaware that this was caused by COVID-19 because they had mild symptoms or none at all,” he said.
Increase in male infertility
Hallak believes COVID-19 can cause an increase in male infertility. Between 15% and 18% of couples have difficulty conceiving, caused by male problems in 52% of cases. This trend may lead to an increase in demand for assisted reproduction, which in his view is sometimes rushed in Brazil, and provided without a properly standardized initial assessment to diagnose the cause. There has to be enough time to work out and propose the approach with the best cost-benefit ratio, including specific treatment to address the cause or restore natural fertile capacity.
“We’ll need to take great care with assisted reproduction in the wake of the pandemic. We don’t know much about the consequences of COVID-19 in the months following infection,” Hallak said.
Because SARS-CoV-2 has been detected in all types of testicular cells, which participate in all stages of spermatogenesis, scientists do not know whether the virus is also present in the sperm of COVID-19 patients months after they recover from the disease. Their sperm may have been affected by the virus, and in Hallak’s view medical teams should wait around 90 days, the time taken by a spermatogenesis cycle, to perform a fresh andrological examination.
“We’ve seen DNA lesions caused by the virus at very high levels of around 80%, whereas up to 25% is considered normal and up to 30% acceptable,” he said.
Another concern is unnecessary testosterone replacement. “If a patient has had COVID-19 and a decline in hormone production is detected, testosterone replacement will further inhibit testicular function,” Hallak stressed. “The testicles have repair mechanisms that restore hormone production, and there are medications that increase natural production of steroid hormones, gradually reestablishing intrinsic testicular function, although we don’t yet know to what extent will it depend on whether Leydig cells have been damaged and how badly.”
“At FMUSP, we are bringing together specialists from various medical specialties to study a group of 749 male patients who had COVID-19 who will undergo a first evaluation over the next four years to obtain more knowledge about the post-COVID-19 syndrome,” says Hallak.
The article “Radiological patterns of incidental epididymitis in mild-to-moderate COVID-19 patients revealed by color Doppler ultrasound” (doi: 10.1111/and.13973) by Felipe Carneiro, Thiago A. Teixeira, Felipe S. Bernardes, Marcelo S. Pereira, Giovanna Milani, Amaro N. Duarte-Neto, Esper G. Kallas, Paulo H. N. Saldiva, Maria C. Chammas and Jorge Hallak is at: onlinelibrary.wiley.com/doi/10.1111/and.13973.
The article “Testicular pathology in fatal COVID-19: a descriptive autopsy study” (doi: 10.1111/andr.13073) by Amaro N. Duarte-Neto, Thiago A. Teixeira, Elia G. Caldini, Cristina T. Kanamura, Michele S. Gomes-Gouvêa, Angela B. G. dos Santos, Renata A. A. Monteiro, João R. R. Pinho, Thais Mauad, Luiz F. F. da Silva, Paulo H. N. Saldiva, Marisa Dolhnikoff, Katia R. M. Leite and Jorge Hallak is at: onlinelibrary.wiley.com/doi/10.1111/andr.13073.
The article “SARS-CoV-2 and its relationship with the genitourinary tract: Implications for male reproductive health in the context of the COVID-19 pandemic” (doi: 10.1111/andr.12896) by Jorge Hallak, Thiago A. Teixeira, Felipe S. Bernardes, Felipe Carneiro, Sergio A. S. Duarte, Juliana R. Pariz, Sandro C. Esteves, Esper Kallas and Paulo H. N. Saldiva is at: onlinelibrary.wiley.com/doi/10.1111/andr.12896.
The article “Viral infections and implications for male reproductive health” (doi: 10.4103/aja.aja_82_20) by Thiago A. Teixeira, Yasmin C. Oliveira, Felipe S. Bernardes, Esper G. Kallas, Amaro N. Duarte-Neto, Sandro C. Esteves, Joël R. Drevet and Jorge Hallak is at: pubmed.ncbi.nlm.nih.gov/33473014.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.




