
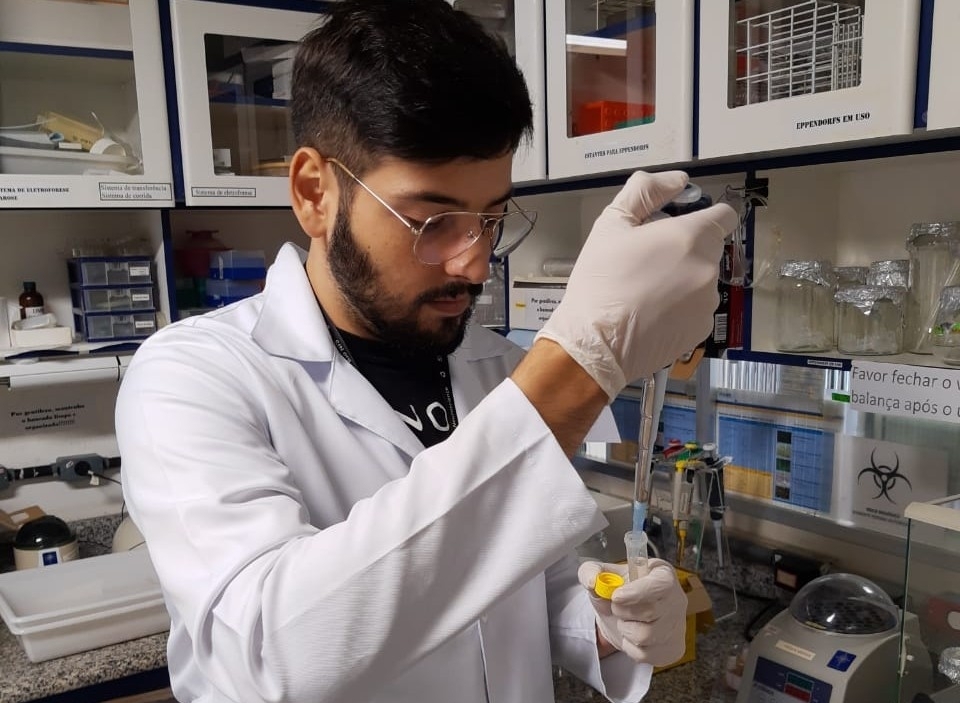
Methodology developed by Brazilian researchers is based on analysis of metabolites in blood serum. Innovation has been patented and reported in Journal of Psychiatric Research (photo: João Victor Silva Nani / UNIFESP)
Methodology developed by Brazilian researchers is based on analysis of metabolites in blood serum. Innovation has been patented and reported in Journal of Psychiatric Research.
Methodology developed by Brazilian researchers is based on analysis of metabolites in blood serum. Innovation has been patented and reported in Journal of Psychiatric Research.
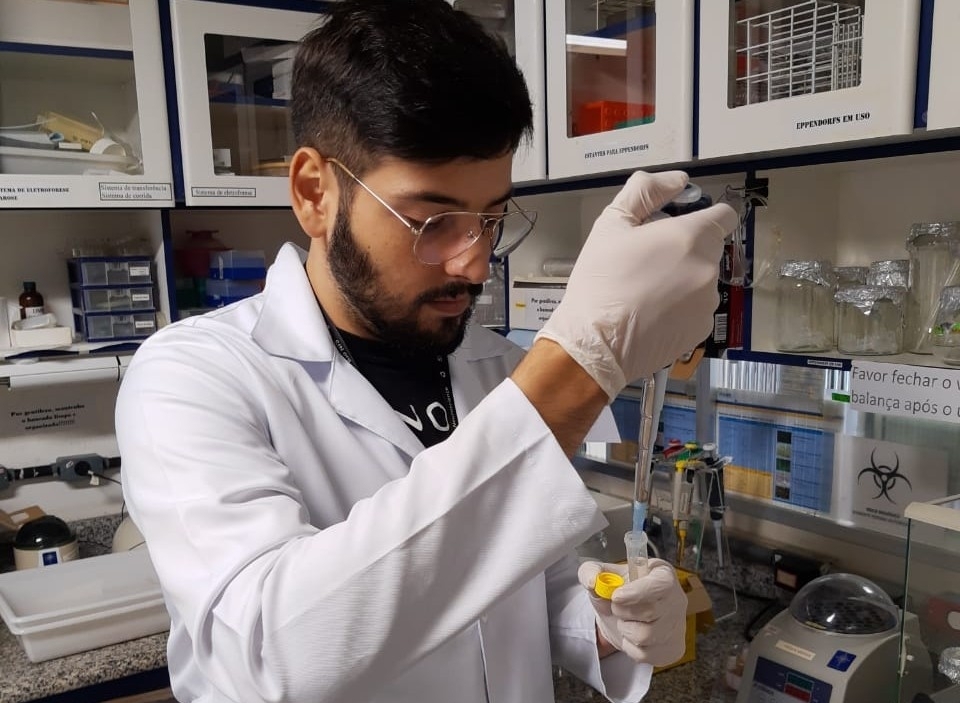
Methodology developed by Brazilian researchers is based on analysis of metabolites in blood serum. Innovation has been patented and reported in Journal of Psychiatric Research (photo: João Victor Silva Nani / UNIFESP)
By Maria Fernanda Ziegler | Agência FAPESP – A methodology developed by Brazilian researchers could permit the creation of a blood test capable of diagnosing two psychiatric diseases with similar symptoms – schizophrenia and bipolar disorder.
Diagnosis of these diseases is currently based on clinical analysis. The process can take years and is highly subjective as it depends on the psychiatrist’s judgment and the patient’s ability to describe symptoms.
The methodology, developed by researchers at the Federal University of São Paulo (UNIFESP) and the University of Campinas (UNICAMP), is the first to distinguish between the two disorders by analyzing biochemical and molecular alterations. The innovation has been patented and is described in a scientific paper published in the Journal of Psychiatric Research.
“It’s complicated to distinguish between two diseases with similar symptoms by clinical examination. Laboratory tests can detect patterns in blood serum and distinguish precisely between schizophrenia and bipolarity, thereby improving the patient’s prognosis,” said Mirian Hayashi, a professor in the Pharmacology Department of UNIFESP’s Medical School (EPM) and principal investigator for the study, which was supported by FAPESP.
According to the researchers, the main innovation of the method is that it analyzes the pattern of metabolites (chemical substances resulting from digestion or other metabolic processes) present in the blood sample, rather than specific biomarkers such as proteins, genes, or other molecules. Blood serum is estimated to contain more than 2 million metabolites.
Previous studies by the group demonstrated the possibility of distinguishing between patients with schizophrenia or bipolar disorder and healthy people.
The researchers also analyzed crack users in light of the fact that crack’s effects closely resemble the first psychotic episode experienced by schizophrenics. “A subject who doesn’t report crack use can be mistaken for a schizophrenic undergoing an initial psychotic episode. In our study, however, perhaps owing to a temporary molecular effect, we were unable to distinguish between drug users and healthy individuals who weren’t drug users,” said Hayashi, who is also affiliated with the National Institute of Science and Technology (INCT) for Translational Medicine, one of the INCTs funded by FAPESP in the state of São Paulo in partnership with the National Council for Scientific and Technological Development (CNPq), a Brazilian government agency.
Distinguishing between cases of schizophrenia and bipolar disorder resulted from the second stage of the research project, which was conducted after the patterns of metabolites had been identified. To prove this distinction was possible using biochemistry techniques, the researchers analyzed blood serum samples from a group of 182 subjects comprising schizophrenic and bipolar patients plus a number of healthy individuals as controls.
As in their previous studies, they had the metabolomic profile of the blood samples analyzed at UNICAMP’s Institute of Chemistry by Professor Ljubica Tasic and her team using proton nuclear magnetic resonance spectroscopy and chemometrics (application of statistics to the analysis of chemical data).
“Our aim was to find different patterns of metabolites and associate them with one of the disorders,” Hayashi said. “To do this we placed the blood serum samples in a magnetic field. Proton nuclear magnetic resonance detects proton peaks in a sample. All molecules contain protons, so it’s possible to produce a resonance profile of fluids with different compositions. Analysis of the variations in protons among different individuals can identify differences in patterns between samples from schizophrenic or bipolar patients and healthy people.”
“The study not only differentiates one condition from the other but also presents new information on both disorders that can be further researched in future. After all, if there’s a pattern of metabolite alterations it derives from a pathway that’s specific to each disease and that so far we haven’t identified,” said João Victor Silva Nani, a co-author of the article with a scholarship from FAPESP.
The discovery of the molecular pathways associated with schizophrenia and bipolar disorder can contribute to the future development of more effective treatments. With this aim, the group has also embarked on a project in collaboration with Japanese researchers that may be funded by the Japanese government.
According to Hayashi, the most widely accepted hypothesis for the main cause of schizophrenia and bipolarity is dopamine imbalance. This is why the main anti-psychotic drugs are dopamine modulators.
“Illegal drugs like crack are known to bring about a short-lived imbalance by boosting the release of dopamine,” Hayashi said. “Crack users tend to manifest similar symptoms to schizophrenics and bipolars when in crisis, which is why we also study them. However, schizophrenics and bipolars also have genetic alterations as well as this chemical imbalance in the brain.”
Using bioinformatics and artificial intelligence, the Brazilian and Japanese researchers now aim to identify the pathways involved in these two disorders. “The genetic reasons for which a subject becomes schizophrenic or bipolar are recognized, but the genes involved are common to several mental illnesses, and if the metabolic pathways exclusive to each disorder can be identified it will be possible to develop more effective therapies in future,” Hayashi said. The researchers are aware that a great deal of research remains to be done before all this can be used in clinical practice and genuinely help patients.
The article “Peripheral biomarkers allow differential diagnosis between schizophrenia and bipolar disorder” (doi: 10.1016/j.jpsychires.2019.09.009) by Ljubica Tasic, Acioly L.T. Lacerda, João G.M. Pontes, Tássia B.B.C. da Costa, João V. Nani, Lucas Gelain Martins, Leonardo A. Santos, Marielle F.Q. Nunes, Marcelo P.M. Adelino, Mariana Pedrini, Quirino Cordeiro, Felipe Bachion de Santana, Ronei J. Poppi, Elisa Brietzke and Mirian Akemi Furuie Hayashi can be retrieved from: www.sciencedirect.com/science/article/abs/pii/S0022395619305205.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.




