
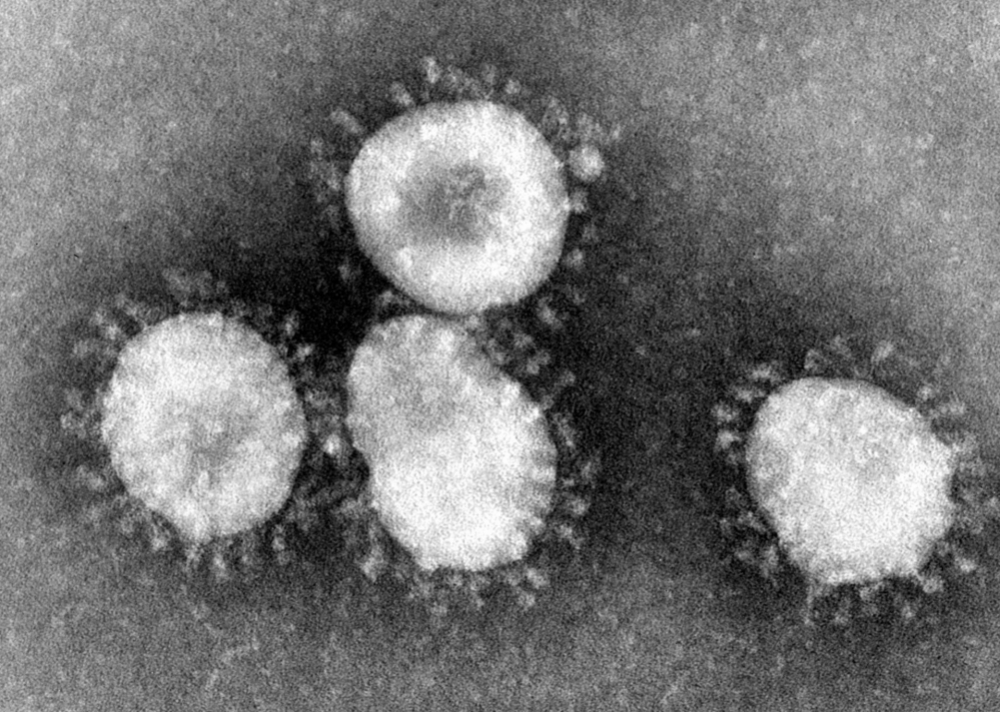
Higher blood glucose levels captured by defense cells provide energy for augmented viral replication, triggering overwhelming immune response that kills lung cells (image: Wikimedia Commons)
Higher blood glucose levels captured by defense cells provide energy for augmented viral replication, triggering overwhelming immune response that kills lung cells.
Higher blood glucose levels captured by defense cells provide energy for augmented viral replication, triggering overwhelming immune response that kills lung cells.
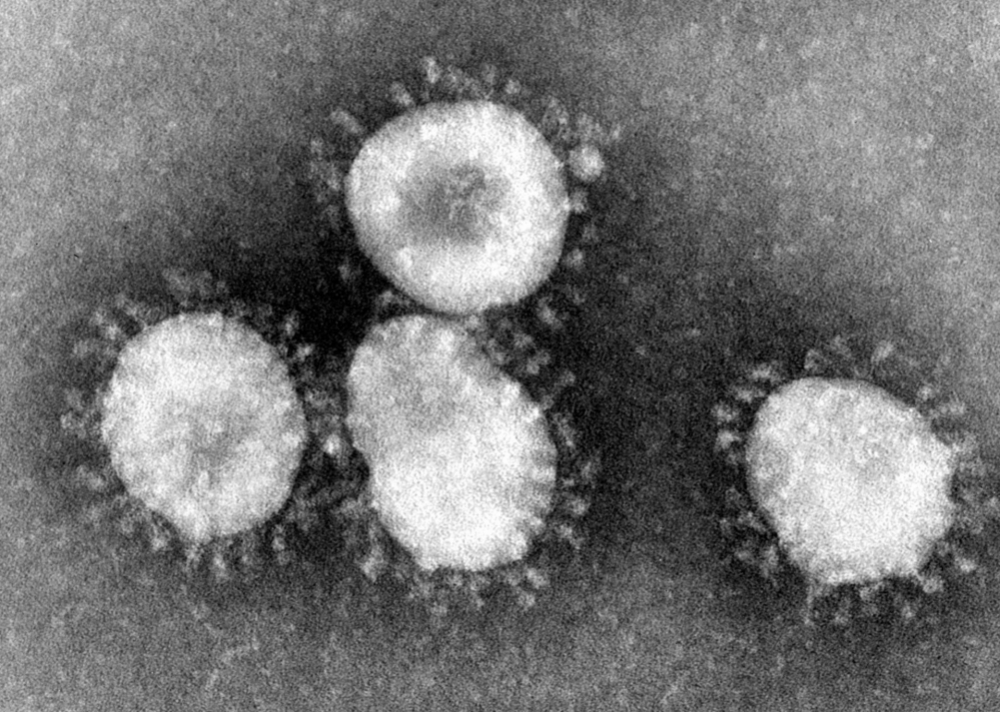
Higher blood glucose levels captured by defense cells provide energy for augmented viral replication, triggering overwhelming immune response that kills lung cells (image: Wikimedia Commons)
By André Julião | Agência FAPESP – Brazilian researchers have discovered one of the causes of severe COVID-19 in diabetic patients. Laboratory experiments showed that the higher level of blood sugar in these patients is captured by monocytes, a type of defense cell, and serves as a source of additional energy for the coronavirus to replicate more than in a healthy organism. In response to the increased viral load, the monocytes release large amounts of pro-inflammatory cytokines with several effects including lung cell death.
The study is supported by FAPESP and led by Pedro Moraes-Vieira, a professor in the University of Campinas’s Biology Institute (IB-UNICAMP) in the state of São Paulo, working with researchers who belong to the university’s COVID-19 task force coordinated by Marcelo Mori, also a professor at IB-UNICAMP.
Mori and Moraes-Vieira are among the authors of an article currently under review for publication in Cell Metabolism and available in a pre-print version that has not been peer reviewed.
“The paper shows a causal link between the increased glucose levels and COVID-19 severity in diabetic patients observed in clinical practice,” said Moraes-Vieira, a researcher with UNICAMP’s Experimental Medicine Research Cluster (EMRC), and also with its Obesity and Comorbidities Research Center (OCRC), a Research, Innovation and Dissemination Center (RIDC) funded by FAPESP and hosted by UNICAMP.
Using bioinformatics tools to analyze publicly available RNA sequencing datasets for lung cells from patients with moderate to severe COVID-19, the researchers observed overexpression of genes involved in the alpha/beta interferon signaling pathway, which is associated with the anti-viral response.
The lungs of patients with severe COVID-19 were also found to contain large amounts of monocytes and macrophages, cells with crucial and distinct roles in tissue homeostasis and immunity.
Monocytes and macrophages were the most abundant cells in the samples. The analysis showed that the glycolytic pathway, which metabolizes glucose, was considerably augmented.
The bioinformatics analyses were performed by Helder Nakaya, a professor in the University of São Paulo’s School of Pharmaceutical Sciences (FCF-USP), and Robson Carvalho, a professor in São Paulo State University’s Botucatu Institute of Biosciences (IBB-UNESP).
Glucose and SARS-CoV-2
The group then performed a series of trials with monocytes infected by the novel coronavirus SARS-CoV-2, in which they were cultured in different concentrations of glucose. The experiments were conducted in IB-UNICAMP’s Emerging Virus Research Laboratory (LEVE), a Biosafety Level III (BSL-3) facility led by José Luiz Proença Módena, a professor in IB-UNICAMP. Módena is supported by FAPESP and a co-author of the article.
“The higher the glucose levels in monocytes, the more viral replication was boosted and the more the defense cells produced molecules such as interleukin-6 [IL-6], interleukin-1 beta [IL-1β] and tumor necrosis factor alpha. All these are associated with the phenomenon known as the ‘cytokine storm’, in which not just the lungs but all other organs are exposed to an immune response flaring out of control and triggering several potentially fatal systemic alterations in severe patients,” Moraes-Vieira said.
The researchers then treated the infected cells with 2-DG, a drug used to inhibit glucose flux. They found that the treatment completely blocked both viral replication and the virus-induced increase in expression of cytokines and ACE-2, the protein used by the virus to invade cells.
They also used 3-PO, a drug that is being tested in patients with some types of cancer. Like certain analogs, 3-PO inhibits the action of a gene involved in the cellular glucose flux. The result of this experiment was less viral replication and less expression of pro-inflammatory cytokines.
The results indicating increased activity of the glycolytic pathway in response to infection were obtained by proteomic analysis of infected monocytes, conducted in collaboration with Daniel Martins-de-Souza, a professor at IB-UNICAMP supported by FAPESP.
Finally, the analyses showed that the mechanism was mediated by the hypoxia-inducible factor-1 alpha pathway, known to be associated with several diseases and to be kept stable partly by the presence of reactive oxygen species in mitochondria, the energy-producing organelles in cells.
The researchers administered anti-oxidants to the infected cells and found that hypoxia-1 alpha activity decreased, ceasing to influence glucose metabolism. This in turn stopped viral replication in monocytes (the infected defense cells), which ceased producing the cytokines toxic to the organism.
“When we intervened in the monocytes with anti-oxidants or drugs that inhibited glucose uptake, we blocked viral replication and reversed the dysfunctionality of T lymphocytes, which are also defense cells, averting the death of lung cells,” Moraes-Vieira said.
The studies with T lymphocytes and the analysis of hypoxia-1 alpha in patients were performed in collaboration with Alessandro Farias, a professor at IB-UNICAMP and a co-author of the published study.
The drugs used in the experiments with cells are currently being tested in clinical trials for treatment of some cancers and can later be tested in COVID-19 patients.
The first three authors of the study are Ana Campos Codo, who has a master’s scholarship from FAPESP; Gustavo Gastão Davanzo, who has a doctoral scholarship from FAPESP; and Lauar de Brito Monteiro, who also has a doctoral scholarship from FAPESP. All three are researchers at IB-UNICAMP supervised by Moraes-Vieira.
“The study was possible only thanks to these collaborations, the commitment of the graduate students who worked day and night on this project, and fast-track funding from FAPESP and FAEPEX [UNICAMP’s Fund to Support Education, Research and Outreach],” Moraes-Vieira said.
The article “Elevated glucose levels favor SARS-CoV-2 infection and monocyte response through a HIF-1α/glycolysis dependent axis” can be retrieved from: papers.ssrn.com/sol3/papers.cfm?abstract_id=3606770.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.




