
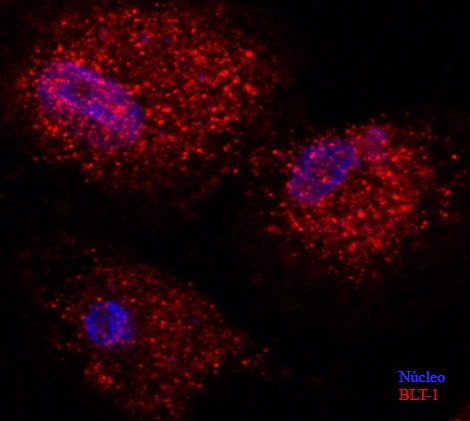
Diabetic mouse macrophages stained by immunofluorescence, with nuclei marked blue and the LTB4 receptor BLT1 marked red (image: Luciano Filgueiras)
A paper published in Science Signaling shows that the inhibition of an inflammatory mediator can reduce sepsis susceptibility in type 1 diabetics.
A paper published in Science Signaling shows that the inhibition of an inflammatory mediator can reduce sepsis susceptibility in type 1 diabetics.
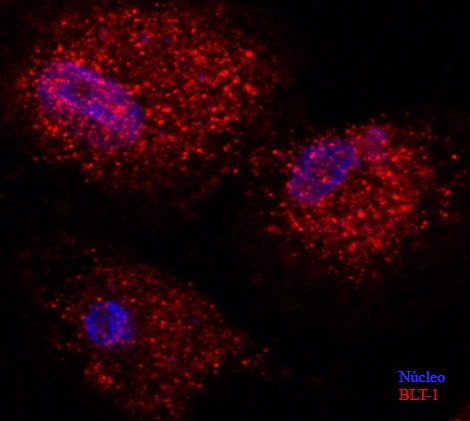
Diabetic mouse macrophages stained by immunofluorescence, with nuclei marked blue and the LTB4 receptor BLT1 marked red (image: Luciano Filgueiras)
By Karina Toledo
Agência FAPESP – A new strategy with the potential to treat sepsis in patients with type 1 diabetes has been proposed by researchers at the University of São Paulo (USP) in a paper published in the journal Science Signaling.
In experiments with diabetic mice, the research group at USP’s Biomedical Science Institute (ICB) achieved a 40% reduction in mortality due to sepsis by treating the animals with a substance that inhibits the synthesis of an inflammatory mediator known as leukotriene B4 (LTB4). Similar drugs are already used to combat asthma and other allergic conditions.
“Our work shows that type 1 diabetic mice present sterile inflammation that is dependent on this mediator, LTB4. This base inflammation increases the susceptibility to sepsis,” said Luciano Filgueiras, the first author of the paper. Inflammation is termed sterile when it is not due to infection.
The experiments were conducted with support from FAPESP during Filgueiras’s PhD research, conducted partly at ICB-USP’s Immunopharmacology Laboratory and partly at Professor Henrique Serezani’s lab at Indiana University – Purdue University Indianapolis (IUPUI) in the United States.
Professor Sonia Jancar, also affiliated with ICB-USP, was the PhD supervisor for both Filgueiras and Serezani.
As Filgueiras explained, type 1 diabetes develops when the patient’s immune system destroys a subset of the pancreatic cells responsible for producing insulin and the level of insulin in the organism thus becomes insufficient to control blood sugar.
Sepsis, sometimes called blood poisoning, is characterized by potentially fatal systemic inflammation that produces changes in body temperature, blood pressure, heart rate, white blood cell count, and breathing. The more severe forms typically cause several organs to malfunction, leading to septic shock.
“Sterile inflammation, which makes diabetics more sensitive to sepsis, is also associated with other diseases such as retinopathy, nephropathy, and atherosclerosis, as well as with impaired healing,” Filgueiras said.
In their study of sterile inflammation in diabetic mice, the ICB-USP research group observed an increase in both levels of LTB4 and expression of a molecule known as myeloid differentiation factor 88 (MyD88) in macrophages, which are white blood cells that are the body’s first line of defense when the immune system identifies a pathogen or an altered cell.
“MyD88 is a key molecule in innate immunity. It’s essential to the intracellular signaling induced by Toll-like receptors, which trigger an inflammatory response,” Filgueiras explained. Innate immunity is naturally present and is not due to prior sensitization to an antigen.
Previous studies by Jancar and Serezani had already showed that MyD88 expression is controlled by LTB4. Filgueiras’s PhD research included an investigation to identify whether high levels of LTB4 cause the sterile inflammation observed in diabetics.
Experiments
The model used by the researchers involved inducing type 1 diabetes in mice by injecting the mice with a drug that destroys insulin-producing pancreatic cells.
“As soon as the animal developed diabetes, it presented an inflammatory condition characterized by the production of pro-inflammatory cytokines and LTB4 as well as by increased MyD88 expression in macrophages. Our next step was to test the response to sepsis,” Filgueiras said.
Sepsis was induced by cecal ligation and puncture (CLP), a procedure that involves puncturing the cecum, part of the large intestine, and allowing feces and intestinal bacteria to spill into the peritoneal cavity.
The mice were divided into three groups: non-diabetics with sepsis, diabetics with sepsis, and diabetics with sepsis treated with an LTB4 inhibitor.
In the untreated diabetic group, 100% of the animals died approximately 24 hours after bowel perforation resulting from systemic inflammation. In the group treated with the LTB4 inhibitor, 40% of the mice survived until the end of the six-day experiment. In the group of non-diabetic mice, the sepsis survival rate was 60%.
Treatment with LTB4 inhibitor was started 16 hours before CLP. A second dose was administered eight hours before the procedure. After CLP, the drug was administered every 12 hours for six days.
In addition to reducing mortality, the treatment also controlled the inflammatory condition, which was evaluated in terms of the production of anti- and pro-inflammatory cytokines.
In another experiment, the researchers evaluated the response to sepsis in mice that had been genetically engineered to not express LTB4 receptors. In this case, both the diabetic and non-diabetic mice displayed a 100% survival rate at the end of the six-day experiment.
“Therefore, in the absence of LTB4 receptors, there was no difference between diabetics and non-diabetics concerning the susceptibility to sepsis,” Filgueiras said. The scientists also compared groups of mice with type 1 and type 2 diabetes. In type 2 diabetes, extra insulin is produced by the pancreas to make up for insulin resistance in fat, liver and muscle cells, which leads to hyperglycemia, although macrophages still respond to insulin.
“The results showed that in the group with type 2 diabetes, there was no increase in MyD88 expression in macrophages, suggesting that this sterile inflammation induced by the LTB4/MyD88 pathway is more closely associated with insulin deficiency than with hyperglycemia,” Filgueiras said.
Therapeutic possibility
According to Filgueiras, drugs capable of inhibiting the synthesis of other types of leukotriene are already used to treat asthma and other allergic diseases.
Substances capable of specifically inhibiting LTB4 are still at the developmental stage and have not been tested for the treatment of sepsis or type 1 diabetes in humans.
“Our research has brought to light a new therapeutic possibility for these experimental drugs. This is important because in the past 50 years, no treatments have been found to significantly increase the survival rate for patients with sepsis,” he said.
The paper was highlighted in the “Editor’s Summary” section of the Science Signaling website.
Filgueiras is currently conducting postdoctoral research with a scholarship from FAPESP and under supervision by Jancar. One of his goals is to test sepsis treatment with LTB4 inhibitors in association with antibiotics.
“We also want to see how LTB4 inhibition could benefit patients with type 1 diabetes more generally – for example, whether it would reduce the incidence of associated diseases such as atherosclerosis as well as of impaired healing,” he said.
This study is part of the Thematic Project entitled “Association of receptors for lipid mediators with PRRs in macrophages and dendritic cells,” for which Jancar is the principal investigator.
“The Thematic Project aims to study the interaction between various lipid mediators such as leukotriene, prostaglandin and platelet activation factors (PAFs) in macrophages and dendritic cells to understand how this alters inflammatory and immune responses,” Jancar said.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.




